Publication Date
3-2025
Files
Download Full Text (317 KB)
Abstract
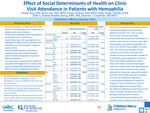
Background Social determinants of health (SDOH) create barriers to seeking care regularly, especially for patients with chronic disease. Patients with moderate-severe hemophilia A and B (factor 8 and 9 deficiencies respectively) have a life-long higher risk of bleeding and require chronic therapies. Specialized care is offered through hemophilia treatment centers (HTCs); however, these can be difficult to access for some individuals. Previous SDOH research in this patient population has been limited; therefore, it can be difficult to identify the barriers to care that exist. There is a need to examine SDOH more thoroughly to create patient-directed interventions to improve access to care. Objectives To identify common SDOH affecting patients with moderate-severe hemophilia and determine how each impacts clinical utilization within a single HTC. Methods A retrospective chart review of patients age < 18 years old with a diagnosis of moderate or severe hemophilia A or B seen at Children’s Mercy Hemophilia Treatment Center over the last five years. Dependent variables included no-show visits, which were any missed visit since the patient established care, and missed yearly comprehensive visits, of which non-parametric distributions were calculated. Rates were standardized to an assumed 10-year follow-up period and then compared across independent variables including race, ethnicity, language spoken, insurance type, rural vs urban home, food insecurity rate, poverty level, distance to an ER and to the HTC using the Kruskal-Wallis and Wilcoxon rank-sum tests, where appropriate. Significant findings were determined using a p-value < 0.05. Results Patients with the following SDOH had a statistically significant difference in rates of no-show visits: distance >60min from the HTC (p=0.009), urban vs rural home county (p=0.033), race of patient (p< 0.001), and insurance status (p=0.007). [Figure 1] Further demographic data and analysis included with confidence intervals provided in Fig 1. Conclusions The rate of no-show visits was most affected by patient race, insurance type, distance from HTC, and urban vs rural living conditions. No statistically significant correlations existed within the yearly comprehensive visits, which may be indicative of the shared importance of keeping regularly scheduled appointments between patient and provider when caring for a chronic disease. Interestingly, though previous data in this field has demonstrated rurality as a limitation to care, these findings suggest that an urban setting closer to the HTC presented more of an issue. These findings also help support the benefits of outreach clinics in providing specialized care directly in rural environments, likely reducing no-show rates in this population. This may inspire a similar approach to localized outreach within the urban neighborhoods affected by SDOH limitations to offer clinics where patients are most vulnerable.
Disciplines
Hematology | Pediatrics
Recommended Citation
Gaur, Shailly; Lee, Brian PhD, MPH; Anderst, James MD, MSCI; Foote, Katie LSCSW, LCSW, OSW-C; Bradley-Ewing, Andrea MPA, MA; and Carpenter, Shannon L., "Effect of Social Determinants of Health on Clinic Visit Attendance in Patients with Hemophilia" (2025). Posters. 444.
https://scholarlyexchange.childrensmercy.org/posters/444




Notes
Presented at HTRS (Hemostasis & Thrombosis Research Society) 2025 Scientific Symposium; March 13-15, 2025; Coronado, California.