Publication Date
11-2025
Files
Download Full Text (325 KB)
Abstract
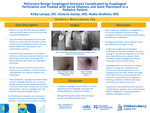
Patient is a 2-year-old male who was originally referred to GI for failure to thrive and recurrent vomiting following feeds. Upper GI showed long-segment stricture with mid-thoracic tapering and initial EGD revealed 2mmx5cm distal esophageal stricture that was balloon dilated with serial dilations and triamcinolone injections. He presented one week after his 3rd dilation with fever, vomiting and respiratory distress and was found to have cardiac tamponade, left pleural effusion, septic shock and esophageal perforation. He was transferred to the ICU and started on broad-spectrum antibiotics, IV fluids and chest tube placement. He required intubation and vasopressors. After stabilization, esophogram showed marked proximal esophageal dilation and no contrast passage into the stomach. Repeat EGD showed recurrence of the severe stenosis but no contrast extravasation. A 10 mm esophageal stent was placed to keep the esophagus patent. Serial EGDs were completed, with mitomycin C application and stents replacements for larger diameters, up to 16 mm, for a total of 3 months. Congenital esophageal stenosis (CES) is a rare but significant cause of dysphagia, aspiration and feeding difficulties in infants and toddlers. Management typically begins with endoscopic therapy with dilation being first line. Other endoscopic modalities in management of CES include endoscopic incisional therapy, esophageal stenting, intralesional steroid injection and Mitomycin C application. Esophageal perforation rates for dilation of CES are reported to be as high as 44.4%. Traditional management of esophageal perforation includes NPO, antibiotics and chest drainage in the setting of large fluid in the chest; which were effective in our patient. Other modalities include esophageal stenting and endoscopic vacuum assisted closure. Esophageal stents can also serve as a bridge to surgery or as long-term management for recurrent strictures though success rate in treating stricture has been variable and ranges from 0-86%. Stents are also associated with numerous complications such as migration, bleeding, perforation, tracheal compression and erosion into adjacent structures. Ultimately this case underscores the need for a multidisciplinary approach, close monitoring and flexible management in managing complex pediatric esophageal strictures.
Disciplines
Gastroenterology | Pediatrics
Recommended Citation
Lampe, Kirby; Sarata, Victoria; and Ibrahimi, Nadia, "Refractory Benign Esophageal Strictures Complicated by Esophageal Perforation and Treated with Serial Dilations and Stent Placement in a Pediatric Patient" (2025). Posters. 491.
https://scholarlyexchange.childrensmercy.org/posters/491




Notes
Presented at the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN) 2025 Annual Conference; Chicago, IL; November 5-8, 2025.