-

Institutional Pilot Changes Lead to a Reduction in Emergency Department Boarding Patients
Rohan Akhouri, Kelly Sinclair, Bethany Bolt, Ashley Daly, Chris Kennedy, and Jennifer Watts
Background:
Crowding and boarding pediatric emergency departments (ED) is an ongoing problem associated with a mismatch in resources and patient care demands. ED boarding can be defined as a patient admitted to an inpatient unit who remains in the ED. ED boarding occurs when there is limited availability of inpatient bed space – either due to patient volume or decreased staffing. ED boarding is associated with adverse events, and increased mortality1. Few studies address the impact of inpatient strategies on ED boarding3,4. The objective of our study was to evaluate hospital-based strategies within a single institution and their effect on ED boarding times.
Methods:
This study was performed at an urban, academic, tertiary-care level 1 trauma center in Kansas City, Missouri. We performed a retrospective analysis of ED boarding times in 2022-2023. Data of total patient volume, and ED boarding patient length of stay (LOS) from January 2022 – September 2023 were collected through the hospital EMR and GE informatics. We compared ED boarding LOS total counts/month before and after implementation of institutional changes, accounting for total ED volume. ED boarders were defined as patients admitted to an inpatient hospitalist or ICU team who remained in an ED room longer than 1 hour. The inpatient strategies began in August 2022 improving communication with ED and floor staff, determining patient medical and social needs for discharge, projected discharge dates, and a rapid room turnover protocol.
Results:
ED patient volume ranged from 6,800-8,000/month and a peak of 12,000 in November 2023. The ED boarding volume decreased from 142 patients in November to zero from January onwards. There was an increase to 40 patients boarded in March 2023. Data up to September 2023 show a continued reduction in ED boarding patients while controlling for total ED volume.
Conclusion:
ED boarding volume decreased after implementation of the hospital-based changes with similar total ED patient volume. Based on our institutional data the inpatient-based systems changes improved communication, planning, and room availability. These changes are achievable and can be implemented in a short period with a reduction in ED boarding, further supporting that ED boarding is a result of inpatient and systemic challenges. The study is limited in its evaluation as more data is needed to compare peak ED visit months and to more closely analyze the impact of the changes.
-
Urinary Melatonin-sulfate in Pediatric Patients with Inflammatory Bowel Disease: A Pilot Study
Moises Alatorre-Jimenez, Kathryn Clarkston, Craig Smail, Norah Almahbub, Craig A. Friesen, and Rachel Chevalier
IBD is widely recognized as a multifactorial condition. Previous research has linked melatonin to IBD owing to its secretion by enterochromaffin cells (EC). Gastrointestinal melatonin serves various functions in the intestine, including activation of membrane receptors such as MT2, modulation of serotonin receptors, regulation of sympathetic neurons, antioxidant properties, and modulation of inflammation. The current study aimed to assess melatonin-sulfate concentrations in spot urines from IBD patients in remission. We hypothesize that the levels of melatonin will be elevated at baseline in patients with IBD in remission due to a chronic inflammatory state.
This study was completed utilizing urine symptoms from a biorepository. In this investigation, a total of 29 spot urine samples were collected from IBD patients in remission (11 female/18 male; mean age 14.4, range 8-20 years; 5 UC/24 CD) and a control group consisting of 29 non-IBD patients (14 female/18 male; mean 14.6, range 8-20 years). Melatonin-sulfate urine enzyme-linked immunosorbent assay (ELISA) was conducted following the manufacturer's instructions (IBL International) to quantify melatonin levels. Melatonin-sulfate concentrations were compared between IBD patients and controls utilizing the Mann-Whitney U test and concentrations were assessed for correlation with ESR and CRP. The effect size was calculated using Cohen’s d.
Urinary melatonin-sulfate concentration was elevated in IBD patients as compared to controls (68.4 ± 142.81 vs. 35.41 ± 42.96; p<0.033). There was a medium effect size (Cohen’s d = .312). There was no correlation between melatonin-sulfate concentrations and either ESR or CRP in either group.
Spot urinary melatonin-sulfate is elevated in IBD patients, even in remission, and is unrelated to inflammatory markers in this group. This is the first study to assess spot urine melatonin-sulfate concentrations and suggests that IBD is associated with altered production and/or metabolism, even in remission. Whether this is reflective of asymptomatic low-grade inflammation is not clear. Although the current pilot study utilized a small sample size, it lays the groundwork for further research into the role for melatonin in the pathogenesis of IBD.
-

Pelvic Asymmetry and Spinal Fixation in Myelomeningocele
Michael Benvenuti, Shanika de Silva, and Lawrence Karlin
Introduction
In patients with myelomeningocele stable low profile pelvic instrumentation required in spinal deformity surgery may be difficult to obtain due to the variable dysmorphic pelvic anatomy. A number of techniques have been proposed but the superiority of one or another in this challenging population has not been established.
Aims/Objectives
Our aim is to determine the pelvic morphology in patients with myelomeningocele associated scoliosis and its relation to pelvic fixation and deformity correction strategies.
Methods
We analyzed the CT scans performed for preoperative planning of scoliosis corrective surgery in 26 individuals with myelomeningocele and the CT scans obtained for the diagnosis of appendicitis in an otherwise healthy age and gender matched cohort. The mean age range was 10.4 years (range 1.9-19.4). Three-dimensional reformatting of the CT scans was performed to permit accurate measurements of bone depth and ideal (best available bone stock) screw trajectories for standard pelvic fixation methods. Segmental anatomic parameters and intersegmental anchor relationships were determined: (1)sacral alar iliac (SAI); (2)posterior superior iliac spine (PSIS); (3)anatomic; (4)sacral-alar; (5) width of sacrum at SAI entry; (6)distance between anchor entry sites.
Results
The cohort of patients with myelomeningocele had greater variation in the angles of their pelvic screws in both the sagittal and axial plane; at least one screw trajectory was impossible in more than half of the myelomeningocele patients compared to only one control patient with an impossible trajectory.
In both groups, the SAI screws (most commonly) had the most harmonious start points compared to L5 screws, however in both groups several patients had L5 start points that lined up better with iliac screws in the horizontal plane. We found that in every patient the sacral ala was at least 1 cm thick and that as a portion of the posterior sacral width, the sacral canal was not wider in the patients with myelomeningocele.
Conclusion
In this cohort of patients with scoliosis and myelomeningocele we found multiplanar pelvic asymmetry that led to wide variation in angles for pelvic fixation and many instances where typical trajectories were not possible due to sacral and pelvic morphology. Three dimensional CT scans are an invaluable aid to the planning of ideal personalized pelvic fixation techniques. Creativity may be necessary with nontraditional screw trajectories or Dunn-McCarthy (or Galveston) techniques to establish a strong pelvic base for spinal fixation and deformity correction.
-
Clinical and gene expression data reveal subtypes of pediatric T-cell acute lymphoblastic leukemia
Meghana Bhumireddy, Irina Pushel, Lisa A. Lansdon, Byunggil Yoo, Midhat S. Farooqi, and Keith August
Background
Acute Lymphoblastic Leukemia (ALL) is a rapidly progressive cancer characterized by excessive immature leukocytes, which transform into leukemic cells and proliferate uncontrollably into lymphoblasts, blocking the production of normal cells. T-ALL constitutes 10–15% of pediatric ALL cases. Unlike B-ALL, T-ALL lacks clinically defined molecular subtypes, hindering risk assessment and treatment determination.
Objective
In this study, we aimed to identify connections between clinical findings and gene expression in pediatric T-ALL to move towards defining more clinically meaningful subtypes of pediatric T-ALL.
Design/Method
We analyzed clinical and gene expression (bulk and single-cell RNAseq) data from eight pediatric T-ALL patients from the Children’s Mercy Research Institute Biorepository. By utilizing various clinical data types (e.g., flow cytometry, FISH, microarray), we identified clinically relevant mutations and gene expression patterns. This offered further insight into characterizing individual patients and establishing related groups of patients.
Results
Our investigation revealed similarities in gene expression involving LEF1, NOTCH1, and RUNX1 among two patients. In the same patients, we also observed T-cell receptor alpha (TRA) rearrangements with TAL and TLX1, indicating consistency between genomic and transcriptome findings. Furthermore, a patient with ETP-ALL had a high proportion of hematopoietic stem cells (HSC)-like cells, while another patient (not classified with ETP-ALL) displayed similar proportions of HSC-like cells and an elevated expression of genes including IL-7 and LMO2 compared to other patients. Moreover, our analysis identified differential expression of ETV6 and TOX across our cohort, providing potential biomarkers for T-ALL subtyping.
Conclusion
Similarities in gene expression patterns among T-ALL patients, even within our small cohort, emphasize the need for refined classifications of distinct subtypes to improve treatment selection and outcomes. Additionally, we found that a patient without clinically defined ETP-ALL criteria shares a similar molecular profile as the patient with Early T-cell Precursor (ETP)-ALL. Patterns of gene and cell surface marker expression offer potential biomarkers for characterizing T-ALL subtypes and prognosis. Furthermore, the diverse signaling pathway activities identified through bulk and single-cell RNA analyses present potential therapeutic targets for treatment strategies. Future exploration utilizing external gene expression datasets is planned to validate findings within the broader context of Children’s Mercy’s cohort of T-ALL patients and lay the foundation for more personalized approaches to diagnosing and treating pediatric T-ALL.
-

The Impact of COVID-19 on the Effectiveness of a Home-based Family Support Program
Danielle Chiang, Stephen Gardner, Emily Siedlik, Emma Sexton, and Donna M. O'Malley
Background: The Team for Infants Exposed to Substance use (TIES) Program is a home-based family support program providing a multi-disciplinary, community-based approach to address the complex needs of families with young children affected by maternal substance use. The TIES Program focuses on six goal areas: maternal drug use, parenting skills, child health, parent health, income stability, and housing stability. This study examines the effectiveness of this home-based program during the peak COVID-19 period of April 1, 2020 – March 31, 2021.
Study Question: How did the COVID-19 pandemic affect parenting practices and child health in the TIES Program compared to those in a matched comparison group?
Methods: Data was collected from 2016 to September 2023. Given the nested structure of the data, we used multi-level models (MLM) and generalized estimating equations (GEE) to estimate the impact of the COVID-19 period on parenting practices and child health goal attainment after controlling for other covariates. Bootstrap procedure was also employed.
Results: We found little impact of the COVID-19 period on TIES participants, but a pervasive and statistically significant negative impact on parenting practices and child health goal attainment from the comparison group. Specifically, results indicated that for the comparison group, the COVID-19 period tended to decrease parenting goal scores by 0.54 to 0.59 units (p<0.001), and child health goal scores by 0.8 units (p<0.001) on scales of 1-5 yet had no statistically significant impact on these two goal areas for the TIES participants. Additionally, of 14 outcome variables analyzed using MLM and GEE, 13 (93%) were negatively impacted during the COVID-19 period in the comparison group, with scores from the comparison group being 5% to 20% lower than those from the TIES Program. Bootstrap results showed similar findings.
Conclusions: The TIES program and its dedicated staff pivoted to provide virtual home visits and employed creative problem-solving to support families during the COVID-19 pandemic. Participation in TIES provided a protective effect for families when compared to those who did not have intensive home-based family support. Home-based family support programs provide vital supportive services in the best of times. Disruption of normal home visiting activities during the pandemic forced programs to think creatively to continue to provide critical services to families that may have otherwise lost access to resources, delayed physical and behavioral healthcare, and experienced severe isolation. The TIES Program demonstrated that virtual modifications in times of emergency can keep families engaged and supported.
-
The Role of Adverse Childhood Events on the Progression of Chronic Kidney Disease in Children: A CKiD Study
Ana Cortez, Bradley A. Warady, Darcy K. Weidemann, John Cowden, and Matthew Matheson
Background
There is a paucity of research on the relationship between adverse childhood events (ACEs) and chronic kidney disease. The effect of ACEs on the long-term health outcomes of cardiovascular disease, cancer, and chronic lung disease first emerged in a paper published in 1998. The National Institutes of Health sponsored the ACE Study, which Kaiser Permanente carried out in California. The study used a 17-question survey addressing seven exposures: psychological, physical, contact-sexual abuse, substance abuse, mental illness, mother being treated violently, and criminal behavior in the household. The results revealed a strong relationship between childhood exposure to ACEs and health outcomes. When individuals experienced four or more such exposures, the odds ratio ranged from 1.6 to 3.9 for ischemic heart disease, cancer, stroke, chronic bronchitis or emphysema, and diabetes (Vincent et al., 1998). This monumental analysis remains a focal point in research more than twenty years after the initial publication of its results. Since then, numerous studies have investigated how childhood exposures can increase disease risk. Surprisingly, chronic kidney disease (CKD) has received little attention in terms of the influence of ACEs in the pediatric and adult populations.
Objective
Specific Aim #1: Characterize the prevalence of ACEs in the CKiD cohort.
Specific Aim #2: Characterize disease progression among those who experienced ACEs compared to those who have not.
Specific Aim #3: Determine if there is a dose-dependent relationship between the number of ACEs and the risk of CKD progression.Design/Methods
Prospective longitudinal observational cohort study:
Stratification by exposure: CKiD participants who reported 1 or more ACEs VS CKiD participants who do not report ACEs.
Primary outcome: CKD progression defined as a composite endpoint of 50% eGFR decline and/or the initiation of kidney replacement therapy (dialysis or transplant).
Inclusion criteria: all CKiD participants with available baseline eGFR and completed questionnaire data regarding ACE exposure. -
Epigenetic drug screen of natural killer cells identified compounds controlling immune training and tolerance
Eric S. Geanes, Elizabeth R. Fraley, Stephen H. Pierce, Rebecca McLennan, and Todd Bradley
Natural killer (NK) cells are cytotoxic innate lymphocytes that provide defense against pathogens and malignancy. New evidence identified that NK cells are capable of memory-like immune responses in certain settings. This innate immune memory is thought to be imprinted through epigenetic modifications. However, precise epigenic pathways or strategies to modulate long-term NK cell activity are not well defined. In this study, we performed a screen of an epigenetic library containing 160 drug compounds with well-characterized epigenetic regulatory mechanisms, to identify drugs and pathways that could train or tolerize NK cell activation. One compound that we identified was the H3K27 methyltransferase Ezh2, which regulated NK cell lineage commitment from bone marrow hematopoietic stem cells and altered the phenotype of differentiated NK cells to increased cytotoxicity. This outcome provides an option to train or induce stronger cytotoxic effects on NK cells. In contrast, another compound we identified was the histone deacetylase inhibitor, Givinostat, which did not alter NK cell commitment from bone marrow stem cells, but significantly decreased NK cell function in the periphery resulting in a more tolerant innate immune state to secondary NK cell stimulation. Identification and exploration of these epigenome altering drugs may offer further insight into downstream pathways of NK cell function or provide novel therapies for tolerizing or priming innate immune responses.
-
Design and testing of mosaic enterovirus vaccine to prevent hand, foot and mouth disease
Gage Greening, Rebecca McLennan, Eric S. Geanes, Santosh Khanal, Oishi Paul, Surya Rangaraj, and Todd Bradley
Enterovirus A (EV-A) has been responsible for recent outbreaks of hand-foot-mouth disease (HFMD); however, there is no vaccine or effective antiviral treatment. The goal of our project is to develop broad vaccines targeting the diverse EV-A serotype viruses that cause HFMD. We used the EV-A viral capsid protein 1 (VP1) as the vaccine antigenic target, because of its genetic diversity across EV-A serotypes, and prior work that showed VP1 has linear neutralizing antibody epitopes. We computationally designed VP1 proteins to create mosaic antigens that optimize B and T cell epitopes among diverse EV-A viral sequences. We identified that a hexavalent mosaic vaccine cocktail had the highest EV-A sequence coverage. We then immunized mice in three groups with recombinant VP1 proteins in adjuvant; Group 1 was given the EV-A Consensus VP1 (Consensus), Group 2 was given the EV-A strain EVA-71 VP1 protein (EVA-71, strain specific) and Group 3 was given our newly designed hexavalent vaccine (EV-A Consensus + 5 mosaic VP1). We measured the antibody binding levels to 9 EV-A VP1 antigens after immunization and found that the EV-A hexavalent vaccine resulted in improved antibody binding breadth during in vivo vaccination. Our results demonstrate the feasibility of using polyvalent VP1 proteins to increase the breath of antibody epitopes among EV-A serotypes. Our approach has the potential to treat and block EV-A infection and serve as a model for responding to other emerging viral diseases.
-

Nursing Knowledge and Confidence Scale
Jeanette Higgins, Sarah Wareham, and Tazim Dowlut-McElroy
Background
Changes in medical practice have led to decreased provider face-to-face time with patients. Healthcare providers are increasingly reliant on nurses to provide patient education during clinic visits. However, lack of knowledge and confidence in educating patients is a significant barrier to the utilization of nurses to enhance the delivery of comprehensive health care by providing health education to patients and families. Postgraduate nursing education is often presented as informal information rather than during dedicated formal education. Formal teaching of disease specific content is associated with increased knowledge and self-confidence which may translate to improved patient education. The aim of this pilot study was to evaluate the effect of formal contraceptive education on nursing knowledge and confidence in the delivery of patient education.
Methods
This was an IRB-exempt Quality Improvement (QI) study at a large metropolitan children’s hospital. A survey with established content validity consisting of 20 questions with responses on a Likert scale (Figure 1) was administered to a convenience sample of nurses within the Division of Gynecology. The survey was administered immediately pre- and post- as well as 30 days after a 1-hour formal educational session delivered by an APRN that included hormonal contraceptive options, instructions on use, and potential side effects (Figure 1). Statistical analysis was performed using SPSS Version 28.0 (IBM Corp, Armonk, NY).
Results
Seventy-five percent of the gynecology nurses (9 out of 12) completed the pre and post surveys, 1 dropped out for the 30-day post survey. There were varying responses regarding confidence about nurses’ ability to answer questions about contraceptive medications, ability to teach medications and review adverse effects with patients/families (Table1). There was an increased confidence with assessing learning, illness and disease states.
Conclusions
Although patient education is a key part of patient care, nurses express varying levels of confidence in teaching patients about hormonal contraception despite formal education. Limitations of this pilot study include small sample size with precluded inferential statistical analysis on the effect on formal teaching on survey responses. Future studies are needed to evaluate factors associated with lack of nurses’ expressed lack of confidence with patient education and the effects of nursing education on patient comfort with use of prescribed hormonal contraception.
-
Key regulators of syncytiotrophoblast cell lineage development in human placentation
Ashley Howard, Keisuke Kozai, Boryana Koseva, Michael J. Soares, Elin Grundberg, and Kaela Varberg
In human placentation, cytotrophoblast cells fuse to form a continuous epithelial cell layer of syncytiotrophoblast (ST). Multinucleated ST cover the villus surface and provide critical structural and biochemical barriers for the developing fetus. ST also produce hormones and growth factors to support pregnancy and promote fetal growth. Despite these critical functions, key transcription factors (TF) and signaling pathways involved in ST differentiation are not fully understood. To identify regulators of ST differentiation, we integrated transcriptomic and genome-wide epigenomic approaches in human trophoblast stem (TS) cells. Human TS cells were maintained in a proliferative stem state or differentiated into ST following a six-day ST3D differentiation protocol. Stem and ST differentiated cells were analyzed using RNA-sequencing, Assay for Transposase-Accessible Chromatin-sequencing, and HiC chromatin capture. Prominent differences in chromatin accessibility, cell transcriptomes and TF binding motifs were identified in Stem and ST cell states. The top ten TF binding motifs identified in ST-specific regions were enriched for AP-1 family members (e.g., Fra1, Fos, JunB, Fra2, BATF, Atf3, Fosl2, AP-1, Jun-AP1), TEAD, and AP-2gamma. Select TFs identified as uniquely enriched in ST cells were localized in human placental tissues by in situ hybridization and mechanistically studied using loss-of-function approaches in the TS cell model. Overall, key regulators of syncytiotophoblast cell lineage development in human placentation were identified.
-

Development of an Isoform Atlas in Pediatric Patients with Rare Diseases using Iso-seq
Boryana Koseva
With the development of next generation sequencing technologies, short-read RNA sequencing became the standard method for rapidly sequencing whole genomes, annotating transcriptomes and quantifying gene expression. However, short-read RNA sequencing can be bioinformatically challenging because the full transcript is inferred from 150 base pair fragments, either by overlapping the sequenced fragments (de novo) or by aligning to a reference genome or transcriptome. The inference of the transcript de novo or through alignment to a reference set make short-read RNA sequencing less than ideal to use in identifying and characterizing the biological diversity of transcripts (isoforms). Recently, full-length (FL) RNA sequencing has been developed in which a single molecule of up to 10 kilobase can be sequenced with high confidence, removing the need to infer the transcript from short fragments. This new approach gives us the ability to discover isoforms resulting from alternative splicing or gene fusion events, as well as detect allele-specific expression and single nucleotide variants. Here, we leverage Iso-seq, the FL RNA sequencing method developed by Pacific Biosciences, to build an atlas of isoforms found in a population (N=81) of pediatric patients with rare diseases across 13 different tissue types. We identified ~2.7 million non-redundant transcripts across ~113 thousand genes. Only 31% of the transcripts were classified as originating from known genes, which means that 69% of the transcripts identified are not in the reference annotation of the human genome. From our preliminary investigation, approximately 47% of transcripts were identified as anti-sense, meaning that the sequenced transcript originated from the non-template strand of the genic region. These observations suggest that there is more biological diversity than short-read sequencing is able to detect. While there is a variety of human-related atlases that are publicly available, our study is the first to undertake the effort to catalog the full complement of isoforms in pediatric patients. Furthermore, we aim to identify tissue-specific isoforms, and highlight the biological diversity of isoforms across tissues.
-

Mapping CHW Community Resource Referral Processes: A Qualitative Study
Lynette Lartey, Emily A. Hurley, Mariah Chrans, Kevin Ochoa, and Helena Laroche
Background: Community health workers (CHWs) are tasked with connecting clients to care and resources, yet the success of these referrals depends on a complex web of factors. This study aims to disentangle the process by which CHWs connect clients to resources and create a process model to guide effective CHW referral systems.
Methods: We conducted a qualitative study guided by the social-ecological model to characterize actions by CHWs to overcome barriers and facilitate successful referrals. We conducted semi-structured interviews with CHWs from two community health organizations. Interviews were transcribed and coded inductively and deductively with Dedoose, with a focus on process coding for the actions occurring during the referral process. CHWs and their supervisor collaborated on the interview guide and recruitment process (two are co-authors).
Results: Interviews (n=16) revealed actions taken by CHW and clients that made referrals successful, including assisting with assessing social needs; eligibility assessment, paperwork, and scheduling; actively communicating with resource organizations; arranging/educating on transportation; accompanying some clients to appointments; following-up; and identifying opportunities to address other health disparities. Themes emerged related to referral facilitators and barriers for client and CHW characteristics, including cultural/language congruency, needs of special populations (e.g., refugees & asylum seekers), coping/stress management, personal relationships with community partners, as well as structural/institutional factors (including efficiency of technology systems, strength of partnership network, availability of resources, and legal/insurance considerations). Mapping the CHW referral processes revealed other actions (e.g., supporting client self-sufficiency, interpreting, & providing emotional support) that CHWs take above and beyond the established processes to facilitate successful referrals. Member checking clarified how these key actions occur throughout the referral process and tied everything together to build trust between the clients and the CHWs.
Lessons Learned: CHWs often take actions above and beyond established processes to make client referrals successful. Enhanced, formalized support of these critical actions will help inform replicable structures to facilitate efficient and effective referral processes.
-
Patient Portal Messaging and Physician Well-Being: A Scoping Review
Sofia Laux, Makayla Ayres, and Thomas Ayres
With the advent of the EMR, physicians have had increasingly more tasks to incorporate into their workflow. In recent years patient portal messaging has become a large component of these EMR related tasks. The effects of EMR workload on physician well-being have been well studied. However, literature is not as robust regarding the specific effect of patient portal messaging on physician well-being. This study aims to review current literature regarding patient portal messaging and its effect on physician well-being. We conducted a scoping review of published literature on patient portal messaging and physician well-being. Relevant keywords were searched on both PubMed and PsycINFO yielding 13,084 articles, 7,965 articles remained after duplicated articles were removed, and 1,893 articles remained after removing articles published prior to 2021. Of the remaining articles, titles were then screened for relevance leaving 50 articles. Abstracts of these 50 articles were screened, leaving 6 full text articles to be reviewed. Conference proceedings from the 2021-2023 International/ American Conference on Physician Health were also reviewed and 1 additional full text article was added. Of these 7 full text articles, 5 met inclusion criteria of being a quantitative study that occurred in the post pandemic era and were included in the final results. Of the articles evaluating this topic, the majority showed a correlation between patient portal messaging and negative effects on physician well-being. Burnout was the most prevalent outcome studied but other indicators of wellbeing varied widely including job satisfaction, feelings of value, heart rate variability indicators of stress, electronic health record confidence or stress, and alignment in values with clinical leaders. Most of these articles examined the amount of time spent responding to patient messages as a predictor of wellbeing. One study also focused on the time of day that responses were made. Another study used natural language processing to conduct a sentiment analysis with no significant results. The results of this scoping review highlight the potential important implication of patient portal messaging and its role in physician burnout. Future research will benefit from examining the use and characteristics of patient portal messages in a post-pandemic era. Specific areas for study include combining length of time and quality of messages as predictors of physician wellbeing.
-

3D Bioprinting the Tumor Microenvironment for Immunotherapy Development
Tykeem Manor, Molly Leyda, John Szarejko, Douglas Myers, and John M. Perry
The tumor microenvironment (TME) is a complex and dynamic system that plays a crucial role in tumor progression, immune evasion, and therapy resistance. The TME is composed of various cell types, including tumor cells, stromal cells, and immune cells, such as macrophages. Macrophages are versatile myeloid cells that can exhibit both protumoral and anti-tumoral functions, depending on their phenotype and the TME context. Classically activated M1 macrophages exhibit proinflammatory and tumoricidal functions and have demonstrated promising anti-tumor effects in immunotherapy research. Conversely, alternatively activated M2 macrophages have wide ranging functions in tissue repair and immune regulation. Tumor associated M2 macrophages (TAMs) are common in the TME where they play a strong anti-inflammatory role and promote tumor immune escape. Understanding the complex interactions between macrophages and the TME is, therefore, essential for developing effective anti-cancer immunotherapies.
The development of immunotherapies typically involves using both in vitro and in vivo tumor models. Classical in vitro 2D models are relatively fast and inexpensive but lack the spatial complexity and heterogeneity of the TME. In vivo mouse models provide a more physiologically relevant system for evaluating the effectiveness of therapies; however, they are time consuming, expensive, and present some significant limitations. Human xenograft models require immunocompromised or humanized mice deficient in several cell types so fail to accurately recreate the TME. 3D bioprinting technology offers a novel approach for creating biomimetic in vitro models of tumors and the TME. By combining the fields of engineering, materials science, and cell biology, 3D bioprinting allows for the rapid and cost-effective creation of complex tissue constructs that accurately mimic the architecture and composition of native tissues. Our research is currently focused on using this technology to recreate the TME by incorporating myeloid, stomal, and tumor cells into 3D bioprinted structures. Utilizing these models, we will investigate the signals which drive the formation of the TME and gain insight on the functions of suppressor cells such as TAMs. Additionally, these models will aid in the development of novel anti-cancer immunotherapies able to evade or repolarize the immunosuppressive TME. We anticipate that our experience creating 3D bioprinted tumor models will facilitate collaborative efforts to screen a wide range of innovative therapies and support translation from bench to bedside.
-

Establishing a Biorepository and Data Bank for Perinatal Research
Brynne Musser, Marc Parrish, Megan Thomas, Shilpa Babbar, Samantha Nguyen, Elin Grundberg, and Michael J. Soares
INTRODUCTION Events and exposures during pregnancy have the potential to adversely affect pregnancy outcomes. Improved infrastructure for the study of pregnancy and pregnancy-related complications is necessary, particularly in the United States where the maternal mortality rate has doubled since 1999. Critical to that infrastructure are maternal, fetal, and paternal biospecimens. We describe the establishment of a perinatal research biorepository (PRB) in the Kansas City (KC) area that biological specimens and related clinical data associated with human pregnancy. Herein we present, lessons learned from enrollment, and the potential for future interdisciplinary research.
METHODOLOGY Principal investigators at Children’s Mercy Kansas City (CMKC) and the University of Kansas Medical Center were responsible for the design and development of the PRB. Biospecimens are collected from The University of Kansas Health System (TUKHS), AdventHealth Shawnee Mission (Advent), and CMKC. Eligible patients must be at least 18 years old, English speaking, and seeking care for reproductive health. Patients are consented during their prenatal clinic visits, and permission is obtained to allow the retention of biospecimens and medical information. Biospecimens are collected after informed consent is obtained and only if the procedure is already indicated for standard care. Biological samples are processed and stored at the CMKC Biorepository (CRIB). Associated clinical data are stored in a secure and confidential database. Investigators who receive samples from the PRB must provide documentation of an IRB-approved protocol and obtain approval by the PRB Scientific Advisory Committee.
RESULTS Since 2018, 1122 families across three KC hospitals have enrolled in the PRB, including 10 who participated during two pregnancies. Maternal age ranges from 18-47 years old. A total of 7151biospecimens have been collected from 744 pregnancies. While 21% of samples are from pregnancies with no complications, the PRB has samples from pregnancies complicated by preeclampsia, gestational diabetes, congenital abnormalities, cancer, autoimmune disorders, substance abuse, and psychiatric disorders.
CONCLUSION The biological samples and clinical data collected by the PRB have the potential to contribute to morphological, biochemical, genetic, genomic, proteomic, metabolomic, and epigenetic analysis, furthering our understanding of the relationship between maternal and fetal health during pregnancy, birth, and beyond. However, the value of the PRB is directly proportional to the diversity of the consented population and the quality of sample collection and storage.
-
Impact of tracheostomy status on sternal wound infections in children following median sternotomy
Rohit Nallani, Brevin Miller, Janelle R. Noel-Macdonnell PhD, Meghan Tracy, Jason R. Brown, James O'Brien, and Daniel R. Jensen
Background: Sternal wound infection (SWI) is a rare but potentially life-threatening complication in children following sternotomy. Risk factors include young age, extended preoperative hospitalization, and prolonged ventilatory support. Few studies have explored the impact of preexisting tracheostomy on SWI in pediatric patients. The purpose of this study is to measure the effect of tracheostomy and other factors on SWI in children undergoing sternotomy.
Methods: A retrospective study was performed of children undergoing sternotomy over a 12-year period at a tertiary children’s hospital. Children with a tracheostomy prior to sternotomy (TPS) were identified and matched by age, height, and weight to children who underwent sternotomy alone (SA). Demographics, medical comorbidities, surgical details, SWI diagnosis and management information, and surgical outcomes were collected.
Results: We identified 60 unique individuals representing 80 sternotomies. The incidence of sternal wound infection was 22.5% (n=9) in children with a tracheostomy and 2.5% (n=1) in those without. The incidence of SWI was greater in children with a tracheostomy (90% vs. 10% in those without, P=0.007) and underlying pulmonary disease (90% vs. 10% in those without, P=0.020). Infections in the TPS group also demonstrated greater frequency of Pseudomonas aeruginosa (n=3) and polymicrobial growth (n=2).
Conclusions: The risk of developing a SWI in children undergoing sternotomy is significantly greater in those with a tracheostomy and underlying pulmonary disease. Further study is needed to understand other contributing factors and ways to mitigate this risk.
-

Implementation of a Remote Software Platform for Pediatric Patients ready to Wean from Tube Feeding: CHAMP for the Feeder
Kristina Nash, Amy Ricketts, Julianne Brogren, Ryan Thompson, Sarah Bullard, Rachel Graham, Sarah T. Edwards, Dana Bakula, and Lori A. Erickson
Background:Remote patient monitoring (RPM) for pediatric chronic conditions promotes proactive healthcare communication and improves the rate of tube feeding (TF) weaning success. Current TF weaning programs have standards of care for data gathering but are reactive, waiting for parents to report through the patient portal or relying solely upon in-person visits. To improve TF weaning, the CMKC’s Interdisciplinary Feeding and Remote Home Monitoring teams have partnered to use the CHAMP® App to support TF weaning. This proposal’s overall objective is to evaluate the impact of the expansion of the CHAMP® App software on TF weaning success at CMKC.
Methods:We conducted a single-site observational study evaluating the success rate (%) and frequency of children (n) that were able to successfully wean from TF (100% of calories by mouth) while maintaining age-appropriate growth using the CHAMP App, compared with those using only a standard outpatient interdisciplinary feeding tube using a tube weaning algorithm (pre-implementation 6-month period) for children aged 1 month to 4 years scheduled in the feeding clinic.
Results: The pre-implementation period (Jan-July 2023) found a tube weaning attempt in 13.8% (17/141) of patients, with 41.2% of those children (7/17) successfully weaning to all calories by mouth. Patients who attempted to wean pre-state were very medically complicated, around 2 years of age, with each having at least one prior hospitalization and they were followed by an average of 6 medical specialties. Weight loss over 10% of baseline weight was the most frequently charted reason for "failed" trial. In a preliminary analysis of the post-implementation group with CHAMP App, 11/2023-Current Feb/2024, 10% (15/150) of children were enrolled, and 100% of those who have completed the study to date (n=9) reached all calories by mouth. Five patients are actively weaning, one is waiting to wean per parent preference, and we continue with study enrollment.
Conclusions: CHAMP® has the potential to revolutionize outpatient TF weaning at CMKC and nationally. We have successfully weaned more children (n=9) in the first 3 months of CHAMP App implementation than the prior 6 months using standard of care TF weaning (n=7). CHAMP® has dramatically improved our team’s capacity for TF weaning and our ability to proactively monitor, communicate, and intervene throughout the TF weaning process. We will continue to recruit for this study and anticipate that CHAMP® will not only improve our success at TF weaning but also dramatically improve patient and family experience.
-

Stability Proteomic Methods To Detect Novel Drug Targets
Whitney M. Nolte, Tomoo Iwakuma, Priscilla Flores-Ascencio, and Alejandro Parrales
Background: The investigation of p53 mutations, prevalent in osteosarcoma (OS), has led to the identification of potential anti-cancer compounds—KU0171032, KU-D2, and KU-D2-F. These compounds exhibit cytotoxic effects in p53-deficient OS cells. We hypothesize that the KU017032 compound series induces reactive oxygen species (ROS) production and inhibits DNA double-stranded break repair by interacting with protein targets, yet the specific proteins binding to KU0171032 remain unclear. Previous targeted experiments including Cellular Thermal Shift Assays (CETSA) suggest a potential interaction between KU0171032 and NBS1, which is crucial for DNA repair. Here, we describe the application of untargeted proteomic methods to identify protein targets of the KU0171032 compound series. Stability Proteomic Methods (SPMs) measure changes to protein stability due to compound binding on a proteome-wide scale using mass spectrometry. Recently these methods have been used to identify the protein targets of small molecules.
Methods: SPMs implemented include Thermal Proteomic Profiling (TPP), Stability of Proteins from Rates of Oxidation (SPROX), Limited Proteolysis (LiP), and Solvent Proteome Integral Solubility Alteration (solvent-PISA). These SMPs quantify compound stabilization/destabilization of protein targets from thermal denaturation, methionine oxidation, proteolysis, and solvent-induced precipitation. The pilot studies involve treating p53-deficient U2OS cell lysates with staurosporine, a pan-kinase inhibitor, and analyzing samples by quantitative liquid chromatography tandem mass spectrometry (LC-MS/MS), revealing thermodynamically stabilized proteins.
Results: OnePot TPP and LiP workflows successfully quantified kinase targets of staurosporine binding. We quantified 2,460 proteins including 6 kinase targets and 3,319 proteins including 27 kinase targets of staurosporine using a OnePot TPP workflow and a LiP workflow, respectively. SPROX, while potentially able to provide good resolution for peptide-level binding events, failed to provide sufficient protein coverage. Thus far we’ve shown that OnePot TPP and LiP are feasible approaches to identify small molecule-protein interactions in OS cells. Analysis of KU-D2-F treated p53-deficient U2OS cell lysates using OnePot TPP and LiP workflows displayed good protein coverage and interesting putative interactions. Ongoing work is necessary to reproduce findings and will be aided by using higher concentrations and reducing batch effects.
Conclusions: This work presents a systematic approach, using staurosporine as a benchmark in piloting SPMs. This allows for the pre-assessment of technique feasibility, emphasizing the potential of OnePot TPP and LiP methodologies in uncovering novel drug targets. Future directions include piloting orthogonal SPMs such as solvent-PISA and further experiments to identify protein binders and better understand the mechanism of the KU0171032 compound series.
-
ECMO Diaries: Can we reduce the symptoms of pediatric PICS through bedside journaling?
Johanna I. Orrick and Sarah P. Jimenez
In the realm of pediatric critical care, advancements in technology and medical interventions have significantly increased survival rates, particularly in Extracorporeal Membrane Oxygenation (ECMO) cases. Children’s Mercy Hospital, a pioneer in pediatric ECMO, boasts consistently lower mortality rates and surpasses international survival benchmarks. However, the success in saving lives has unveiled a new challenge – Post Intensive Care Syndrome (PICS) in children.
PICS, defined in 2010 for adults, manifests as new or worsening long-term comorbidities, affecting cognitive, psychological, social, and physical aspects, persisting after an intensive care stay. With up to 88% of pediatric patients demonstrating psychological issues post-ICU, the younger the child at admission, the more profound the impact. Pediatric ECMO survivors are particularly vulnerable, with increased risks correlated to the severity of illness, resuscitation requirements, length of stay, and invasive procedures.
Recognizing the escalating prevalence of PICS among pediatric ECMO survivors, the Children’s Mercy ECMO team initiated a research project focusing on implementing ICU diaries as a potential intervention. The project aims to bridge the gap in PICS research for children, acknowledging the unique challenges they face in psychological recovery compared to adults.
Drawing inspiration from successful ICU diary programs in adult ICUs, the project introduces ECMO-specific customized diaries led by ECMO Registered Nurses (RNs) and Respiratory Therapists (RTs). These diaries serve as a tool to document a patient's progress, illness narrative, and daily occurrences, fostering communication between the healthcare team and families.
Focusing on ensuring feasibility, the project addresses concerns about patient privacy, liability, and long-term sustainability. The diary project involves ECMO staff as exclusive writers, providing a structured entry guide to maintain consistency. Diaries are transferred to families upon completion of the ECMO run, ensuring the hospital is not responsible for their maintenance.
Having obtained Institutional Review Board (IRB) approval, engaged Family Advisory Board Members, consulted legal experts, and secured funding, the project is poised for implementation. The initial phase will assess the diary project's effectiveness in mitigating PICS symptoms among pediatric ECMO survivors and their families.
Anticipating success, the team envisions expanding the project to include non-English options and extending its application to diverse pediatric populations beyond ECMO. Sharing the results through conferences and journals, they hope to contribute valuable insights to the broader pediatric critical care community, emphasizing the potential of ICU diaries in improving outcomes for young intensive care unit survivors.
-

Pediatric Caregiver Perspectives on Immigration Status in the Healthcare Setting
Anik Patel, Alison L. Fowler, Juan S. Farias, Ana Contreras, Claudia Zepeda, Estefania Bazan, John Cowden, Frances Turcotte Benedict, Jennifer Watts, and Kimberly Randell
BACKGROUND:
Although the full impact of family immigration status on children’s health in the US is poorly understood, there are known barriers to healthcare access for the country’s approximately 11.4 million undocumented immigrants. Understanding parent/caregiver knowledge, attitudes, perceptions, and beliefs about how their own and their children’s immigration status affects their children’s ability to live a healthy life with adequate healthcare supports may help identify opportunities to improving immigrant children’s well-being.
OBJECTIVES:
This study aims to 1) explore pediatric caregiver knowledge, attitudes, and beliefs regarding impacts of immigrant status on healthcare and 2) describe health and social needs of families for whom one or more caregivers has undocumented immigration status and preferred methods for resource connections among undocumented caregivers.
METHODS:
In this qualitative study, we are interviewing and administering an online demographic survey to up to 30 caregivers attending a pediatric health visit. Inclusion criteria are Spanish-speaking, Latin/Hispanic caregivers who are 18 years and older and have no social security number. Enrollment began April 2023 (16 interviews completed to date, with a goal of 20 total). Data is collected anonymously. Interviews are conducted with a qualified bilingual interpreter and are audio recorded, then transcribed and translated verbatim. We are using an inductive, thematic analysis approach. Each transcript is coded independently by 2 team members. The 3-member coding team meets regularly to iteratively refine the interview guide and codebook, resolve coding discrepancies through transcript review and discussion, and identify data saturation. Codes will be organized into themes and subthemes, then refined by the full study team, which includes practicing clinicians, qualitative methods experts, medical Spanish interpreters, and a native Spanish-speakingculture and language coach. We will summarize demographic data will be summarized with descriptive statistics. We will complete interviews and data analysis by March 2024.
RESULTS:
Coding is currently in process, but early themes include fears related to immigration/immigration status, logistics of disclosure (to whom to disclose to, where to disclose, etc.), how to increase comfort with disclosure, how immigration status effects access to resources, and what resources immigrant families need in the Kansas City area. These will be refined, analyzed, and summarized by March 2024.
-

Neighborhood Walking Environments Around Bus Stops: A Community-Based Participatory Approach for Streetscape Data Collection
Madison Pilla, Cory Yeager, Lauren Fitzpatrick, Chelsea Steel, Amanda Grimes, Jannette Berkley-Patton, and Jordan A. Carlson
Background: Streetscape-level neighborhood walking conditions may impact access to public transit and opportunities for healthy lifestyles. However, little data are currently available about these factors for streets within Kansas City, MO (KCMO).
Objective: This project engaged community members to collect information about streetscape features surrounding bus stops in KCMO neighborhoods. Data collected from this project was disseminated back to community members to support planning and foster advocacy amongst KCMO communities.
Methods: Community members were recruited and trained to serve as “Citizen Scientists” by conducting walk audits of KCMO streets surrounding bus stops. Walk audits were conducted using a tool adapted from the Microscale Audit of Pedestrian Streetscapes (MAPS) tool and examined features related to street segments (blocks), intersections, and bus stops. The tool covered constructs such as street and land use, street infrastructure, bus stop amenities, aesthetics and social characteristics, and perceptions (e.g., safety). Audit routes began at a bus stop and traveled 4 blocks in multiple directions surrounding the stop toward the nearest residential and commercial areas.
Results: In total, 36 Citizen Scientists participated in training and certification to conduct walk audits. Audits were completed for 257 bus stops and 318 walking routes. 29% of walking routes near bus stops had poor sidewalk quality, 77% of intersections on street blocks that had a bus stop had poor crossing quality, and 44% of bus stops had poor quality amenities (e.g., no sidewalks (8%) and/or no lighting (28%)). Additionally, Citizen Scientists reported feeling “unsafe” while walking on 17% of street blocks audited. Maps were created for 11 high-poverty KCMO Zip Codes to indicate the quality of the specific sidewalks, crossings, and bus stops audited. Following data collection, Citizen Scientists engaged in a community advocacy event to share the information collected and lessons learned with other community members and leaders.
Conclusions: The community-based approach of this project was feasible for completing a large number of walk audits across KCMO and enabled community members to engage in data-driven advocacy for their neighborhoods. The community advocacy event was attended by city leaders who engaged with Citizen Scientists about their work. Neighborhood conditions varied highly across neighborhoods and low-income neighborhoods had several barriers to pedestrian safety.
-

Respiratory Syncytial Virus (RSV) Transmission in Household Settings
Montserrat Santos, Anjana Sasidharan, Trina Regis, Kelly Fatheree, Manjusha Rani, Dithi Banerjee, and Rangaraj Selvarangan
Background and aim: Children play a significant role in the transmission of respiratory viruses within households and communities. This gives significance to pediatric studies in how they can provide insight about transmission within households. There are currently a limited number of RSV transmission studies in family clusters conducted in the USA. We aimed to monitor the spread of RSV in prospectively enrolled families and determine viral shedding from multiple specimens in index child (IC) and their household contacts (HHC).
Method: Children (>1 month and <18y) who tested positive for RSV at Children’s Mercy Hospital, and their HHCs were consented to provide demographic and clinical data. Multiple specimens such as nasal swab (NS), saliva (SA), stool (ST), and blood (B) from IC and HCC were collected over 3 weeks. Nucleic extractions were performed, and RSV RT-PCR was done on the samples from the different time points for viral detection.
Results: Overall, 3 families with 12 subjects (3 IC and 9 HHC) were enrolled between Feb 24- current. Median age for all subjects was 5 years (range: 0.3 - 46 years; interquartile range [IQR]: 22- 1.7 years). Median age for IC was 1.5 years (range: 0.3 - 2 years; IQR:1.75 -0.9). Among IC, all three were Black African American. Among the 12 subjects, 9 (75%) subjects had RSV detected in at least one sample, with positivity rates of 42% (5/12) in NS, 58.3% (7/12) in SA; RSV was undetected in ST. The mean Ct values for pediatric samples were 25.4 for NS and 34.9 for SA, Ct values for adult NS and SA were 33.2 and 37.4 respectively. None of the IC had prior exposure to an RSV positive adult HHC.
Conclusions: Viral detection rates differ among specimen types and current preliminary data shows that viral load was higher in NS than SA in both children and adults. Additionally, RSV transmission within the enrolled households possibly occurred from children to adults and more data is needed to infer the secondary attack rate of infection. RSV subtyping RT-PCR and digital PCR will be performed in the future to determine the RSV subtypes and viral load in the samples.
-
Improving Appointment Show Rates in a Pediatric Feeding Clinic: A Descriptive Analysis of Pre-intervention
Ryan Thompson, Kristina Nash, Amy Ricketts, Julianne Brogren, Sarah Bullard, Rachel Graham, Alexandra Zax, Sarah T. Edwards, Keith Feldman, Dana Bakula, and Lori A. Erickson
Background: Children with medical complexities are surviving with the added medical needs of tube feeding weaning. In 2022, 45% of 1549 new or follow-up visits were not attended (19% no-show/26% cancellation) for children 0-3 years of age in the Interdisciplinary Feeding Clinic (IDC). This current care model faces challenges in accommodating the rising volume of referrals, exacerbated by persistent no-shows. We are undertaking a quasi-experimental study with a pre-post-intervention design to address this. This proposal aims to identify patient characteristics associated with missed appointments in the IDC.
Methods: We conducted a retrospective chart review on patients scheduled for feeding appointments within the pre-intervention timeframe of January to July 2023. The patient list was solicited from the HealtheAnalytics administrative database. The data extracted from the EMR was meticulously collected, managed, and transcribed into REDCap. Demographics and clinical and administrative data were reviewed for mean (SD), median (IQR), and incidence (%). Patient characteristics were divided into two groups, attended and not attended, and then compared for differences across groups.
Outcomes: The pre-intervention analysis revealed 1513 appointments with an average no-show rate of 13.53%, lead time to the scheduled appointment of 84.11 days, and a cancellation rate of 15.98%. Of those appointments, 487 patient MRNs met inclusion for retrospective review, with 69.8% (340) patients in the attended appointments group. Patients that attended were most often those with prescribed medications and had a history of emergency room visits for feeding needs, but there was not a significant difference across groups for those that had enteral feeding needs. While there were differences across groups by parent-reported race, this needs to be evaluated cautiously due to sample frequency. There was a higher rate of attendance when the lead time was shorter (61 days vs. 76 days).
Conclusion: There is significant room for improvement in patient access within CMH IDC, and there are multiple options to target to improve access. Lead time to the first appointment with the clinic is the most significant predictor of attendance at a visit during the study period, suggesting that initial access to the IDC should be the primary target for intervention. Improving overall access to the clinic by increasing the treatment success rate for common concerns such as tube feeding weaning (i.e., CHAMP implementation) may help improve show rates by reducing lead time.
-
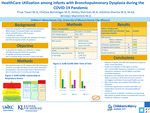
Health Care Utilization among Infants with BPD during the COVID-19 Pandemic
Priya Tiwari, Chelsea Borntrager, Ashley K. Sherman, Jotishna Sharma, and Winston M. Manimtim
Background: Infants with bronchopulmonary dysplasia (BPD) have long-term pulmonary sequelae. These infants continue to require high level of care after discharge from the neonatal intensive care unit (NICU). Limited data exist on the health care utilization of infants with BPD discharged from the NICU during the Covid-19 pandemic.
Objectives: To determine the health care utilization of infants with BPD after NICU discharge during the Covid-19 pandemic. Secondly, to identify risk factors associated with increased health care use.
Methods: Retrospective study (2019-2021) of infants with BPD (n=139) followed in multidisciplinary high-risk clinic. Demographics, respiratory support and co-morbidities were collected during the first, 6-month and 12-month follow-up visits. At each visit, subjects were assessed to have their respiratory symptoms under control (SUM score 0), partially controlled (1) or uncontrolled (2). Health care utilization is defined as acute respiratory events leading to one or more of the following: hospitalization, ED visit, sick clinic visit, use of antibiotics or use of systemic corticosteroids. A score of 1 is assigned for each event for a maximum respiratory event score of 5. Poisson regression model was used to determine the association between the SUM score and acute respiratory events. Repeated measure of logistic regression model was used to determine variables that are associated with increased health care utilization.
Results: Table 1 summarized the demographic and clinical characteristics of the cohort. During the pandemic, subjects with uncontrolled symptoms had 3 times the rate (95% CI 2.3 – 4.2) of having respiratory event compared to those who were partially controlled, and 32 times (95% CI 20.80 - 50.97) the rate of those under control. Acute respiratory events as measures of health care utilization were similar for all infants with BPD regardless of the severity of the disease (mild vs moderate, or mild vs severe, p=0.911 and p=0.263). Subjects with BPD-associated pulmonary hypertension had 3 times odds of higher health care utilization compared to those without pulmonary hypertension, p=0.023, OR 3.05, 95% CI (1.17-7.96).
Conclusion: During COVID-19 pandemic, infants with BPD whose respiratory symptoms are uncontrolled were more likely to have acute respiratory events that require health care use. Infants with BPD had increased health care utilization regardless of disease severity. BPD-associated pulmonary hypertension is an additional risk factor associated with increased health care utilization.
-

Postnatal Dexamethasone for Evolving BPD in Infants on Chronic Non-Invasive Respiratory Support
Priya Tiwari, Jansynn Radford, Michael Norberg, and Alain Cuna
Background: Postnatal dexamethasone (DEX) has traditionally been reserved for preterm infants on prolonged mechanical ventilation, with reported rates of successful extubation at 47% to 76%. Recent emphasis on avoiding mechanical ventilation has resulted in preterm infants being increasingly supported with chronic non-invasive ventilation (NIV). The use of DEX for weaning preterm infants on chronic NIV remains largely unexplored.
Objective: To determine efficacy of postnatal DEX in weaning infants on chronic NIV, and to identify factors and outcomes associated with successful weaning.
Methods: Single-center retrospective study (2010-2022) of preterm infants ≤32 weeks gestation treated with postnatal DEX while on chronic NIV. Data on baseline demographics, respiratory characteristics at start and end of treatment, and clinical outcomes were collected. Primary outcome was rate of successful weaning from NIV to high-flow nasal cannula (HFNC). Other outcomes included factors and outcomes associated with successful weaning.
Results: A total of 56 infants (mean gestational age 26 weeks, mean birth weight 890 grams) received postnatal DEX while on NIV. The average postnatal day and postmenstrual age at time of treatment were 78 days and 37 weeks, respectively. DEX treatment resulted in a significant decrease in oxygen and ventilation support from baseline to end of treatment (Fig 1). Overall, the rate of successful weaning to HFNC was 46% (26/56). Infants treated with postnatal DEX for the first time had similar rates of successful weaning compared to infants who had received prior DEX treatment (43% vs 39%, P =0.79). Factors associated with successful weaning to HFNC were earlier age and lower NIV and oxygen support at time of DEX treatment (Table 1). Infants with successful weaning were more likely to be discharged earlier with less bronchopulmonary dysplasia and less retinopathy of prematurity compared to infants with unsuccessful weaning (Table 2). Other complications of prematurity were similar between the two groups (Table 2).
Conclusion: In our level IV NICU, efficacy of postnatal DEX to wean infants on chronic NIV was 46%. Our results suggest that DEX may also be useful in infants on chronic NIV, but further studies are needed to fully determine efficacy and safety.
-

Exploring the Role of Pain on Physical Activity among Youth with Acute Lymphoblastic Leukemia using the Biopsychosocial Model
Anna van Asselt, Renee Gilbert, Meghan Tokala, Jacee Weber, Meredith Dreyer, Robert C. Gibler, and Carolyn R. Bates
Introduction: Engaging in physical activity (PA) during cancer treatment benefits a child’s physical and mental well-being (McLaughlin et al., 2021). However, engaging in PA may be challenging due to treatment and disease-related pain (Uhl et al., 2020). Pediatric cancer research has primarily focused on management of procedural and chronic pain, with fewer studies examining how pain may interfere with PA during treatment (Clews et al., 2022). The current study qualitatively investigated the impact of pain on PA using a biopsychosocial framework in a sample of youth with acute lymphoblastic leukemia (ALL).
Method: Caregivers (N=17) of a child diagnosed with ALL within the last 12-months and on active treatment completed a semi-structured interview about perceptions of their child's health behaviors during ALL treatment. This analysis focused specifically on discussion of their child’s PA and sedentary time. Thematic analysis followed Braun and Clark’s 6-step framework (2006) to identify themes of caregiver-reported barriers to engaging in PA through a biopsychosocial lens.
Results: Caregivers identified several ways pain impacted PA across the biopsychosocial framework. Key pain-related barriers included: reliance on child’s motivation to be active (psycho/social), distress around seeing their child in pain when resting and being active (social), and fear of interfering with medical equipment (bio/psycho/social). Despite these barriers, caregivers discussed finding creative solutions to adapt activities for their child (e.g., playing with bubbles in bed) (bio/social). Notably, caregivers readily adhered to advice from their medical team. However, caregivers reported that medical advice around PA was highly variable.
Conclusions: The relationship between pain and PA during ALL treatment is complex and influenced by biological, psychological, and social factors. Future directions include understanding factors influencing medical advice on safe and appropriate levels of PA during treatment and supporting caregiver distress to promote child PA during ALL treatment.
-

No-Show Clinic Appointments and the Social Determinants of Health in Pediatric Patients with 22q
Adrian Williams, Antonio Bon Nieves, Meghan Tracy, and Jill M. Arganbright
Introduction: 22q11.2 deletion syndrome (22q11DS) and 22q duplication syndrome present a wide range of medical challenges. The health and well-being of pediatric patients with 22q11DS may be influenced by socioeconomic factors, which can significantly shape their healthcare experiences, access to services, and overall quality of life. The objective of this study is to identify what factors are correlated with no-show clinic visits for children with 22q11DS.
Methods: A retrospective chart review was performed on pediatric patients in a 22q patient registry of a tertiary care facility that includes patients with 22q11DS and 22q duplication syndrome. Demographic data, sex assigned at birth, appointment attendance, comorbid conditions, and patient specific outcomes were collected for analysis. The patient’s home address was cross-referenced with the GeoMarker database to define corresponding specific socioeconomic contextual variables.
Results: 236 patients were included in the study including 198 patients (83.9%) with 22q11DS and 38 patients (16.1%) with 22q duplication syndrome. Collectively, these patients were scheduled for a total of 9,734 clinic visits and 2,347 visits with the 22q multidisciplinary clinic. The overall mean rate of no-show clinic visits was 7.69% ± 10.90. Factors associated with clinic no-show included lower median household income (OR (95% CI) 1.43 (1.25-1.64), p < .001), lower fraction of population with high school diploma (OR (95% CI) 2.33 2.04-2.67), higher fraction of population below the poverty line (OR (95% CI) 1.52 (1.32-1.73), p < .001) and higher fraction of population that required assisted income (OR (95% CI) 1.38 (1.21-1.58), p < .001). Interestingly, farther distance from the tertiary care facility was associated with lower no-show rate (OR (95% CI) 0.71 (0.60-0.85), p < .001).
Conclusion: These findings highlight the potential influence of socioeconomic factors on no-show clinic appointments in pediatric patients with 22q11DS. These factors can be used to help identify patients at risk of no-show clinic appointments and be used to develop targeted interventions aimed at improving clinic attendance and ultimately elevating patient outcomes.
-

The use of Tranexamic Acid for control of post-tonsillectomy hemorrhage in the pediatric population
Adrian Williamson, Macaulay Ojeaga, Meghan Tracy, Jill M. Arganbright, and Elie Khalifee
Introduction: Tonsillectomy is a common surgical procedure, frequently performed to address recurrent tonsillitis, obstructive sleep apnea, and other related conditions. Despite its routine nature, post-tonsillectomy bleeding remains a significant concern. This study explores the role of Tranexamic Acid (TXA) in the management of post-tonsillectomy bleeding.
Methods: A retrospective chart review was performed on pediatric patients at a tertiary care facility who presented with postoperative tonsillectomy hemorrhage from March 2023-June 2023. Demographic data, sex assigned at birth, comorbid conditions, medication administration, and patient specific outcomes were collected for analysis.
Results: 41 consecutive patients were included in this study. The mean age for this preliminary data collection was 7.86 ± 4.32 years. Of the 41 patients, 32 received nebulized TXA while 9 did not. Of the patients that received nebulized TXA, 9 patients (28.1%) returned to the OR for control of bleeding while 23 patients (71.9%) had resolution of bleeding without surgical management. Of the patients who did not receive TXA, 4 patients (44.4%) returned to the OR for control of bleeding.
Conclusions: In this preliminary study, the use of nebulized TXA appears to be associated with a lower rate of return to the operating room for control of post-tonsillectomy bleeding in pediatric patients. While the sample size is limited, these initial findings suggest a potential benefit of TXA administration in reducing the need for surgical re-operation following tonsillectomy. Further research is needed to support these observations and establish the optimal dosing and administration protocols for TXA in this context.
-

Development of an E-cigarette & Tobacco Use Intervention for Adolescents and Young Adults in the Pediatric Hospital
Shelbie Wooten, Melissa K. Miller, Kimber Richter, Karen Wilson, Delwyn Catley, and Abbey R. Masonbrink
Background The pediatric hospital represents a valuable opportunity to identify and treat e-cigarette use among adolescents and young adults (AYAs). However knowledge on how best to provide this care is lacking. We aim to fill this gap by developing and preliminary testing an intervention to treat e-cigarette use among hospitalized AYAs.
Methods We enrolled AYAs (14-21 years) admitted to a pediatric hospital who reported past 30 day e-cigarette use. We offered an evidence-based intervention including education, motivational interviewing, and quit plan development by a health educator and pharmacotherapy prescription by a physician. We used previously developed survey items (multiple choice, Likert scale items) to assess demographics, e-cigarette use behaviors, nicotine dependence, motivation and confidence to quit at baseline and post-intervention. We also assessed intervention acceptability and feasibility using 5-point Likert scale items. Descriptive statistics were used to calculate proportions, means and standard deviations (SD).
Results Of 334 AYAs approached, 68 (20%) were eligible and enrolled (i.e., reported past 30 day e-cigarette use). The mean age was 16.3 years (SD:1.3), forty-six (68%) were female, and thirty-six (53%) had government insurance. Forty (59%) reported occasional use (<9 e-cigarette use>days), six (9%) were more frequent users (10-19 e-cigarette use days) and twenty-two (32%) were regular users (20-30 e-cigarette use days). The mean nicotine dependence score was 7.9 (SD:5.3; low dependence). Compared to baseline the sufficient knowledge to quit increased (22% to 52% [p=0.004]) and confidence to quit increased post-intervention (39% to 70% [p=0.004]). Twenty-five (46%) committed to a quit plan, thirty-two were eligible for pharmacotherapy (47%) and seven were prescribed pharmacotherapy (13%). Forty-eight AYAs were somewhat to very satisfied with the intervention (89%) and fifty-three rated the information as mostly to very helpful (98%). Thirty-six (67%) somewhat to strongly agreed that being in the program was minimally disruptive to their clinical care.
Conclusions Preliminary testing indicates our intervention is feasible and acceptable and may have positive effects on motivation, confidence and quit plan initiation. AYAs agreed the intervention was acceptable and not disruptive to clinical care. We will continue enrolling until our pilot study n=144 is reached, findings may change with the larger sample size. Future work is still needed to further develop evidence-based treatment of e-cigarette use, including nicotine dependence and marijuana co-use, in this population.
-

Assessing Reach of Family-Based Behavioral Treatment for Pediatric Childhood Obesity Offered through Primary Care
Cory Yeager, Jordan A. Carlson, Denise Wilfley, Lisa Nelson, Meredith Dreyer, and Sarah Hampl
Background: Obesity disproportionately affects children from low-income families, highlighting the need to improve treatment reach for this population. Family-based behavioral treatment (FBT) is an evidence-based multicomponent intervention to aid families in making pragmatic and impactful changes.
Objective: To assess the reach of FBT in two health systems serving low-income families.
Methods: FBT was implemented in rural Freeman Health System (FHS) and urban Children’s Mercy (CM) pediatric practices. Eligible patients included children ages 5-12 years with a BMI percentile ≥95th enrolled in Missouri Medicaid. The study was only offered in English. Patients were recruited through provider referrals during clinic visits or directly (letters/calls from intervention team). Patient reach was calculated by comparing the number and representativeness of referred and enrolled patients to all eligible patients and logistic regression was performed.
Results: 18.4% and 8.6% of eligible patients were referred to treatment in FHS and CM, respectively, with a higher proportion of providers in FHS (100%) making referrals than in CM (40.0%). Referral rates varied across providers, with FHS providers referring an average of 17.4% (standard deviation [SD]=8.3%) of eligible patients and CM providers referring an average of 10.9% (SD=24.2%) of eligible patients. Respectively at FHS and CM, 25.6% and 56.6% of referred patients enrolled in treatment, whereas only 5.8% and 9.5% of those recruited directly enrolled. Thus, referred patients were significantly more likely to enroll in treatment than patients recruited directly (FHS OR=4.15, 95% CI=2.15, 8.08, p<.001; CM OR=12.30, 95% CI=6.58, 23.58, p<.001). Latinx patients, in particular, were more likely to enroll via referral than via direct recruitment. 22% and 38% of patients enrolled via referral were Latinx, whereas 10% and 26% of patients enrolled via direct recruitment were Latinx, in FHS and CM respectively, though these differences were non-significant (FHS OR=2.50, 95% CI=.428, 14.6, p=0.281; CM OR=1.70, 95% CI=0.65, 5.571, p=0.357).
Conclusion: Although only a small proportion of eligible patients were referred to FBT by their primary care provider, provider referrals supported reach by increasing enrollment among patients. Encouragement from primary care providers may be valued highly by some patient families, and this may be especially true in certain population subgroups such as Latinx families. More work is needed to improve understanding of barriers to provider referrals to pediatric obesity interventions and to identify strategies for facilitating referrals that minimize burden on providers.
Printing is not supported at the primary Gallery Thumbnail page. Please first navigate to a specific Image before printing.



