Files
Download Full Text (305 KB)
Publication Date
5-2024
Abstract
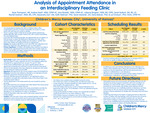
Background: Children with medical complexities are surviving with the added medical needs of tube feeding weaning. In 2022, 45% of 1549 new or follow-up visits were not attended (19% no-show/26% cancellation) for children 0-3 years of age in the Interdisciplinary Feeding Clinic (IDC). This current care model faces challenges in accommodating the rising volume of referrals, exacerbated by persistent no-shows. We are undertaking a quasi-experimental study with a pre-post-intervention design to address this. This proposal aims to identify patient characteristics associated with missed appointments in the IDC.
Methods: We conducted a retrospective chart review on patients scheduled for feeding appointments within the pre-intervention timeframe of January to July 2023. The patient list was solicited from the HealtheAnalytics administrative database. The data extracted from the EMR was meticulously collected, managed, and transcribed into REDCap. Demographics and clinical and administrative data were reviewed for mean (SD), median (IQR), and incidence (%). Patient characteristics were divided into two groups, attended and not attended, and then compared for differences across groups.
Outcomes: The pre-intervention analysis revealed 1513 appointments with an average no-show rate of 13.53%, lead time to the scheduled appointment of 84.11 days, and a cancellation rate of 15.98%. Of those appointments, 487 patient MRNs met inclusion for retrospective review, with 69.8% (340) patients in the attended appointments group. Patients that attended were most often those with prescribed medications and had a history of emergency room visits for feeding needs, but there was not a significant difference across groups for those that had enteral feeding needs. While there were differences across groups by parent-reported race, this needs to be evaluated cautiously due to sample frequency. There was a higher rate of attendance when the lead time was shorter (61 days vs. 76 days).
Conclusion: There is significant room for improvement in patient access within CMH IDC, and there are multiple options to target to improve access. Lead time to the first appointment with the clinic is the most significant predictor of attendance at a visit during the study period, suggesting that initial access to the IDC should be the primary target for intervention. Improving overall access to the clinic by increasing the treatment success rate for common concerns such as tube feeding weaning (i.e., CHAMP implementation) may help improve show rates by reducing lead time.
Document Type
Poster
Recommended Citation
Thompson, Ryan; Nash, Kristina; Ricketts, Amy; Brogren, Julianne; Bullard, Sarah; Graham, Rachel; Zax, Alexandra; Edwards, Sarah T.; Feldman, Keith; Bakula, Dana; and Erickson, Lori A., "Improving Appointment Show Rates in a Pediatric Feeding Clinic: A Descriptive Analysis of Pre-intervention" (2024). Research at Children's Mercy Month 2024. 17.
https://scholarlyexchange.childrensmercy.org/research_month2024/17