-
Addressing Moral Distress: A Call To Action For Nursing
Angie Knackstedt and Cathy Cartwright
Nursing is caring and complex, committed to patients and families, as well as the profession and society. Nurses experience the stress of witnessing pain, suffering, and injustices that violates their moral values – personally and professionally – creating moral distress. Moral distress is the experience of not being able to act in accordance with one’s core values, the feeling that it is nearly impossible to do so or that one’s actions did not result in the intended outcome due to institutional constraints. Over time if moral distress is not mitigated, it has a crescendo effect that can lead to burnout, poor mental well-being, decreased quality patient care and job satisfaction, or the intent to leave a position or the profession.
This poster will discuss evidence from the MMD-HP survey of Children’s Mercy APRNs and their collaborating physicians and address moral distress and ways to mitigate it through ethical and organizational resources.
-

Analysis Of A Cystic Fibrosis-Specific Antibiogram Before And After Fda Approval Of Elexacaftor/Tezacaftor/Ivacaftor (ETI)
Kathryn Bohannan, Claire Elson, and Jane Beyer
The highly effective cystic fibrosis transmembrane conductance regulator (CFTR) modulator elexacaftor/tezacaftor/ivacaftor (ETI) was FDA approved in 2019. Yearly cystic fibrosis-specific antibiograms at Children’s Mercy – Kansas City were analyzed pre-ETI approval (2018-2019) and post-ETI approval (2020-2021) to evaluate differences in susceptibility to antibiotics and the prevalence of selected microorganisms.
-
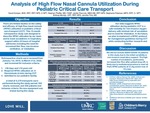
Analysis Of High Flow Nasal Cannula Utilization During Pediatric Critical Care Transport
David Kemper, Stephen Pfeiffer, Jenifer Pannullo, Stephanie Petersen, Brittney Montijo, Brian Lee, and Jennifer Flint
OBJECTIVE: This 15-month retrospective study was designed to describe high flow nasal cannula (HFNC) utilization by our critical care transport (CCT) team and to track escalations in respiratory support within 24 hours of hospital admission. METHODS: Data was collected from January 1, 2019, to March 31, 2020; 6,279 pediatric transports completed during this time. Inclusion criteria: >30 days and < 18 years old, required HFNC ≥ 4 L/min during transport, and admitted to CMH. SARS-COVID-19 patients were excluded. All patients used standard high flow equipment; no new equipment trialed. We tracked high flow status based on if the transport team initiated the device, the referral initiated it but the team weaned it, or if the referral initiated it but team continued the settings. RESULTS: 382 charts reviewed; 358 patients met inclusion criteria. Median age 0.7 years old, with an interquartile range (IQR) of 0.3-1 year of age. Median weight 8.4 kilograms (kg), IQR 6.2-11 kg. Median transport time 80 minutes (min), IQR 69-115 min. Most of our HFNC volume was initiated by the referral (78%). We transported (59%) back to the PICU and (41%) to Peds. Median HFNC 10 L/min with an IQR of 6-15 L/min appreciated at drop-off regardless of HFNC status (initiated by transport, weaned by transport, or continued referral settings) (p-value 0.122). Escalations of care were tracked up to 24 hours after patient drop-off. A total of 118 patients (33%) had an escalation of care; 90 (76%) required an increase in flow, 28 (24%) required non-invasive ventilation, and 0 (0%) required intubation within 24 hours. Escalations typically occurred within the first 6 hours after patient drop-off, 96 (27%), with a median HFNC 10.25 L/min, IQR 8-14 L/min. DISCUSSION: The number of PICU admissions was likely due to our institutions HFNC floor criteria: < 2 years of age, no comorbidities, suspected respiratory viral illness, max 2 L/kg and/or 15 L/min, ≤ 40% FiO2. The high number of escalations in liter flow after patient drop-off (~25% of high flow volume) was likely due to inpatient protocol to initiate at 2 L/kg or max of 15 L/min. In the future, we plan to implement a HFNC protocol for management guidelines during CCT while conducting further research and review. CONCLUSION: Our data suggests HFNC utilization in pediatric CCT is a safe modality for non-invasive oxygen delivery with minimal risk of escalation and no need for intubation.
-
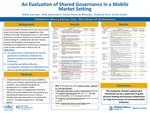
An Evaluation Of Shared Governance In A Mobile Market Setting
Shelly Summar, Matt Kleinmann, Evelyn Donis De Miranda, Kimberly Pina, and Emily A. Hurley
Background:
Community health initiatives across the country seek ways of ensuring community engagement. One method is through shared governance, an alternative to more traditional governance structures, like a board of directors, that aims to promote a mutual understanding of the collaborative decision-making process. Children’s Mercy designed a shared governance framework for decision-making around healthy eating and active lifestyles and applied it to a recent food access initiative in a low-income community in Kansas City, KS. Our objectives were: 1) to explore how a framework for shared governance facilitates collaborative decision making in community health initiatives; 2) to identify and define effective participatory methods of collaboration for use in a revised governance framework.
Methods:
A Mobile Market Community Council (MMCC) was established to guide the development of a mobile market to increase food access. The MMCC was made up of over a dozen community members, including resident members, organizational members, and neutral members (facilitators). The MMCC was introduced to our shared governance framework. The Wilder Factors of Collaboration Inventory (WCFI) measured collaboration among the group with a 5-point Likert scale (1= “Strongly Disagree to 5= “Strongly Agree) to evaluate 44 statements across 21 Collaboration Factors. It was administered at baseline (May 2018) and project end (fall 2019).
Results:
Across all Collaboration Factors, 82% of responses were rated as either “agreed” or ‘Strongly Agreed’. A large increase was seen over time in perceived collaboration across 10 statements (e.g. from ‘Agree’ to ‘Strongly Agree’), and a decrease in 2 statements. The largest improvement was the statement, “Each of the people who participate in decisions in this collaborative group can speak for the entire organization they represent, not just a part” (average score at baseline-=2.7, at project end=4.0). The highest scoring statement was, “The people in this collaborative group are dedicated to the idea that we can make this project work”, (4.9) and increased by 0.7 between the two surveys. Other statements that scored highly were, “Everyone who is a member of our collaborative group wants this project to succeed” (4.9), and “This group has the ability to survive even if it had to make major changes in its plans or add some new members in order to reach its goals” (4.8).
Conclusion
This evaluation showed a governance framework can be a useful tool to guide decision making and increase collaboration for long term success of community health initiatives.
-

A New Surgical Technique For Salvage Of Post-Operative Proximal Junctional Failure In Pediatric Patients–A Case Series
Mason Fawcett and Richard M. Schwend
Background: PJF is a known complication following posterior spinal fusion surgery and can be most simply defined as any adverse event necessitating surgical revision of the proximal instrumentation of the spine. PJF is associated with pain, decreased neurologic function, infection, and increased morbidity. Very little literature exists on this topic in children or on specific surgical techniques for revision surgery.
Methods: The revision technique involves extending the spine instrumentation proximally with paired sets of sublaminar bands used as anchors. The bands are gradually and sequentially tightened, bringing the spine into a corrected sagittal position. Patients who underwent this procedure and had at least two years of follow-up were identified. Demographic and clinical data, as well as plain radiographic and CT sagittal spine parameters were analyzed before the surgery and at the most recent follow-up.
Results: Eight children, average age 14 years, 10 months, were included in the study with an average follow-up time of 31 months. The revision surgery occurred approximately three years following the initial surgery. There was 20° (ranging from an increase of 18° to a decrease of 46°) mean kyphotic angle correction at the site of the failure and 16° (ranging from an increase of 24° to a decrease of 78°) mean cervical lordosis correction, utilizing an average of 6 bands. Before revision, all patients reported neck/upper back pain, with rod prominence. At the most recent post revision visit, pain was markedly reduced, and rod prominence had resolved. One patient reported an increased satisfaction with appearance, and another noted that maintaining horizontal gaze was easier.
Conclusion: Children who received this surgical technique for their PJF experienced resolution of pain and upper rod prominence and improved cervical spine sagittal radiographic parameters that was maintained at 2 years after revision surgery.
-

A Novel Approach To Operating Room Readiness For Airborne Precautions Using Simulation-Based Clinical Systems Testing
Nichole M. Doyle, Todd A. Glenski, Chris Kennedy, Rachael L. Pedigo, and Alyssa Stoner
Introduction:
COVID-19 resulted in major challenges to our global health systems. We had to develop clinical protocols to care for COVID-19 patients with a very short window for design and deployment. We hypothesized that in situ simulation-based clinical system test (SbCST) could help identify latent safety threats (LSTs) in the newly developed protocols for COVID-19 patients in the operating room. The primary outcome was the number of LSTs identified. The secondary outcome was the perceptions of staff related to the process collected via post-training survey data.
Methods:
This observation study took place in the CMH OR and was approved by the IRB. Prior to arriving participants were instructed to review the COVID protocol and watch the training video that had been developed. Each participant began as the assistant and then participated as the airway manager for the next scenario. Short debriefs reviewed guidelines, and gathered staff input, and then staff repeated the simulation to consolidate learning. After completion each participant completed a brief survey to evaluate for knowledge gained, feasibility, acceptability, and suggestions for improvement. Members of the department then completed a follow up survey 4 months later.
Results:
A total of 14 anesthesia staff completed the training. A total of 17 unique LSTs were identified. A resolution was found for all LSTs. (Table 1)
In all, 12 participants filled out the post debriefing survey. All strongly agreed it was worth their time. 92% strongly agreed and 8% somewhat agreed that this was an acceptable way to improve system readiness and staff knowledge and that this was an effective way to test changes and provide feedback. All participants strongly agreed that the debriefing process allowed them to share their ideas for improvement.
Discussion:
We found that in situ simulation is a good way to prepare for disease outbreaks and test the development of new protocols. It allowed for the practice of care team dynamics within the actual clinical environment. It also enabled us to identify and address unexpected problems that were not obvious during the formulation of the protocols. Based on the staff perceptions this method was highly rated and worth the time it took.
Conclusion:
In situ simulation of our COVID-19 protocols allowed us to identify and address problems not foreseen during the planning stages and led to many downstream changes to the protocol. It improved participant compliance and increased their confidence with the new process.
-

A Screen For Therapies For Vici Syndrome, A Rare Neurodegenerative Disorder Of Autophagy
Julia Draper, Vivien Drummond, Scott Weir, and Jay L. Vivian
Vici Syndrome is a devastating genetic pediatric disorder with complex clinical phenotypes. Affected children exhibit profound developmental delay, seizures, hypotonia, immunodeficiency, cardiomyopathy, and progressive loss of motor function, with a median survival of 42 months. This recessive genetic disorder is caused by deleterious variants in the EPG5 locus. This gene encodes a critical component of the intracellular machinery which couples autophagocytic material to the lysosome for degradation. In the absence of EPG5 function, autophagy is impaired, resulting in selective and progressive neuronal and other cellular damage leading the complex phenotypes of Vici Syndrome. VS is thus a member of an expanding class of diseases, termed congenital disorders of autophagy, in which deficits in autophagy are believed to be the underlying driver of the disease. There are essentially no treatment options for children with Vici Syndrome.
Therapies are desperately needed to enhance and extend the quality of life of these children. The overarching long term goals of this project are to identify small molecules that enhance autophagy for use in treatment of this devastating disorder, in a precision therapeutic effort. In this study we are taking a transdisciplinary approach to identify and validate novel therapies for Vici Syndrome. Our team has generated novel cell and animal models in an effort to recapitulate the relevant molecular, cellular, and whole animal aspects of the disease.
VS patient-specific induced pluripotent stem (iPS) cells from two VS patients and an unaffected sibling have been reprogrammed in our lab. Each of these lines were engineered to carry a reporter for autophagy amenable for high throughput screening and analysis of autophagocytic defects. A initial high throughput screen of FDA approved compounds was performed on undifferentiated iPS cells. Our initial efforts have identified several compounds that enhance autophagy and warrant further study. Further screens will be performed on cardiomyocytes and neurons differentiated from the engineered iPS cells.
In a parallel effort, two novel mouse models of Vici Syndrome have been recently engineered using genome editing to recapitulate two clinically identified deleterious variants of EPG5. Future studies in these models will include assessment of viability and deficits in autophagy, to confirm their utility as a disease model and to define the baseline of phenotypes. We will also initiate testing of the drug hits that have come out of our drug screening efforts.
-

B Cell Receptor Repertoire Dynamics And Convergent Evolution Following Sars-Cov-2 Vaccination
Elizabeth Fraley, Santosh Khanal, Cas LeMaster, Stephen Pierce, Tomi Pastinen, and Todd Bradley
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a novel betacoronavirus causing Coronavirus disease 2019 (COVID-19). B cell receptors (BCRs) are expressed at the surface of the B cell and are secreted as soluble antibodies. These antibodies can block viral infection by neutralizing the virus, are critical for resolution of SARS-CoV-2 infection and may be correlates of protection for COVID-19 vaccines. We have previously shown that SARS-CoV-2 immunization elicits a robust antibody response that is significantly higher in individuals who recovered from COVID-19. Moreover, recovered individuals had slower antibody decay in their levels seven months after vaccination. Here, we sequenced the BCR repertoire of individuals undergoing vaccination by SARS-CoV-2 mRNA vaccine (Pfizer, BNT162b2) with (seropositive) or without (seronegative) previous laboratory confirmed COVID-19 infection. We identified genetic differences in the BCR repertoire between groups including V gene usage, CD3R length, percentage of somatic hypermutation, and clonotype diversity. We then focused our analyses to vaccine-expanded clonotypes in both groups to further analyze the differences in BCR repertoire on candidate SARS-CoV-2-specific clonotypes. We determined the frequency of pre-existing clones present after infection that were engaged by the vaccine in the seropositive group. Moreover, in both groups we identified clonotypes that were shared among individuals that could be a result of convergent evolution. Defining the characteristics and evolution of the BCR repertoire during vaccination of individuals with different histories of viral infection will aid in understanding SARS-CoV-2 humoral response dynamics.
-

Budesonide Embedded Sodium Alginate Thin Films For Controlled Release To The Esophagus
Norah Almahbub, Jacob Vandervaart, and Rachel Chevalier
BACKGROUND: Eosinophilic esophagitis (EoE) is an allergic inflammatory disease affecting children at an increasing rate leading to poor weight gain, vomiting, esophageal strictures and increased health care burden from repeated endoscopies. Oral budesonide is the only drug commercially available for treatment, but adverse effects and compliance limit its utility.
We seek to design a microscale, low-aspect ratio, biodegradable, dispersible form of budesonide with controlled release. Our first step is to fabricate thin films utilizing common mucoadhesive polymers (chitosan and sodium alginate) embedded with budesonide. Here we report on the release characteristics of these thin films.
METHODS: Budesonide is suspended in 5% w/v sodium alginate (NaAlg) in water. Using a spin coating method, we first deposit a thin film of 0.25% chitosan to improve wettability. We then deposit a thin film of budesonide/NaAlg solution on silicon wafers. Finally, calcium chloride (CaCl2) solutions of 50 mM, 100 mM, and 400 mM are deposited in the same manner to allow for NaAlg crosslinking. The final film is approximately 1.5-2 µm thick measured with profilometer. The chitosan contributes negligible thickness and the CaCl2 step does not change the thickness of the NaAlg layer. After spin coating the film, we measured a 3cm x 3cm square of the film and removed it from the wafer using a razor blade. The square was placed in 5 mL of artificial saliva at 37°C and 1 mL samples were removed at time points 1 min, 10 min, 20 min, 30 min, and 40 minutes. One mL of fresh saliva was replaced to keep the volume at 5 mL. Budesonide concentration in the samples was measured using UV high performance liquid chromatography (HPLC).
RESULTS:
All concentrations of CaCl2 resulted in a thin film that was easily handled and pliable (Figure 1). All three crosslinked films maintained the majority of their structural integrity for the duration of the drug release study. Significant breakdown of the films was not seen until around 1 hour in saliva. The lower concentration of CaCl2 for crosslinking resulted in faster release of the budesonide into the surrounding saliva (Figure 2). However, all concentrations show a steady, controlled release profile.
CONCLUSIONS:
We have successfully fabricated budesonide embedded NaAlg thin films with controlled release characteristics. Our next steps to make microscale thin films (microdiscs) and evaluate how the low aspect ratio and mucoadhesive properties affect esopahgeal retention.
-

Cervical Necrotizing Fasciitis And Shock In The Post-Operative Pediatric Patient: A Case Report
Paul Hankey and Jason R. Brown
Objectives: Cervical necrotizing fasciitis (CNF) is a rare infection that can quickly lead to devastating patient outcomes. Considering the vital importance of surrounding neck structures, rapid control of the infection is essential to ensure favorable patient outcomes. Infection is most frequently polymicrobial and occurs in the adult patient in the context of certain medical comorbidities. Complications are typically limited to tissue destruction in the form of necrosis. There are no current reports describing CNF complicated by acute shock in the post-operative pediatric patient.
Methods and Results: We present a pediatric case of CNF complicated by acute shock following Sistrunk procedure for removal of a supposed thyroglossal duct cyst.
Conclusions: This case illustrates a potential post-operative complication that can be seen within the pediatric patient. Although most reported examples of CNF are polymicrobial and result from odontogenic infection, providers should be aware of other potential sources of disease. It is important for the pediatric surgeon to rapidly identify CNF and consequent shock, as prompt medical and surgical interventions are critical to offering the best chance of patient survival.
-

Characteristics Of Hospitalized Children Associated With Restraint Use At A Free-Standing Children’s Hospital
Adrienne DePorre, Vincent S. Staggs, Ingrid Larson, Ashley Daly, and Cy Nadler
Introduction:Hospitalized children are at risk for agitation and behavioral dysregulation, which may escalate to unsafe behaviors. If less restrictive de-escalation strategies fail to mitigate serious safety risks to self or others, mechanical restraints may be used on a limited basis. Restraint use, however, is problematic due to associated negative child mental health outcomes and injury risk. Pediatric studies of restraint use outside of dedicated psychiatric facilities are lacking. Specifically, clinical and demographic features associated with restraint use are poorly described. A broader understanding of restraint use among hospitalized children can guide alternative strategies for management and restraint mitigation efforts.
Objective: To describe clinical and demographic features of children associated with mechanical restraint use for unsafe behaviors.
Design/methods: We conducted a single-center, retrospective cohort study of patients 5-20 years of age hospitalized during 2017-2021 at our free-standing children’s hospital, which has no associated psychiatric or behavioral health units. We identified restraint encounters by electronic medical record query of physician orders and nursing documentation. Relative risk of restraint was modeled as a function of patient and hospitalization characteristics using a mixed Poisson working model with a random intercept to adjust for clustering of hospitalizations within patients; length of stay was included an exposure variable.
Results: We included 29,964 patients (46,853 encounters), including 221 patients (271 encounters) with associated restraint use. Based on model results, restrained patients tend to be older and to have higher sex- and age-adjusted weight z-scores, and were more likely to be male, have public insurance, and receive general pediatric care vs. surgery or specialty care (Table 1). Risk of restraint was lowest among Hispanic patients and highest among Black patients. Nearly two-thirds (63%) of patients experiencing restraint had a coded behavioral health diagnosis at some visit during the study period.
Conclusions: We observed strong associations between specific clinical and demographic characteristics and the use of restraints during hospitalizations, and our results suggest racial disparities in restraint use. Our results may inform interventions to reduce unnecessary restraint use and improve health equity. Multicenter studies describing health disparities in restraint use, as well as variation in restraint use and associated clinical outcomes are needed.
-

Decoding The Transcriptional Programs Governing Natural Killer Cell Memory Establishment
Stephen Pierce, Santosh Khanal, Rebecca McLennan, and Todd Bradley
Natural killer (NK) cell memory can be established in response to short-term stimulation with myeloid-derived cytokines, specifically, IL-12, IL-15, and IL-18. Memory NK cells have been shown to produce more interferon-gamma and display higher cytotoxic function upon re-challenge, compared to unstimulated NK cells, much like adaptive cytotoxic T-cells. Memory NK cells have been demonstrated to display increased killing of leukemic tumor cells and are currently in clinical trials for cancer cellular therapy. Other recent studies have also identified that memory NK cells expand in response to infections, such as tuberculosis and HIV-1. However, it remains unclear the precise transcriptional programs that govern the transition of NK cells to memory NK cells and how this this long-term cellular phenotype is preserved. Here, we utilized single-cell RNA-sequencing (scRNA-seq) to study the dynamics of the transcriptome of NK cells during memory establishment. We stimulated human peripheral blood NK cells from five distinct donors overnight with the myeloid cytokine cocktail, or a basal amount of IL-15 as a control, and performed scRNA-seq at two, three- and eight-days post-stimulation. We observed alterations in metabolic genomic signatures, including an upregulation of reduction-oxidation transcripts associated with oxidative stress mitigation in the primed samples at days two and eight, indicating key changes in metabolic pathways. Defining the NK cell transcriptome during memory establishment will reveal potential targets for exploitation during vaccine design against pathogens such as HIV-1, or to overcome barriers related to immunotherapy. Our findings define novel transcriptional trajectories for memory NK cell differentiation up to one week post exposure and suggest that resting memory NK cells readily express metabolic machinery associated with enhanced cytotoxic function and cytokine secretion.
-

Development, Implementation, And Evaluation Of A Simulation Based Educational Curriculum Targeted For Pediatric Hospitalists
Lisa Carney, Matt Hall, Kayla R. Heller, and Chris Kennedy
Background: In 2010, Pediatric Hospital Medicine (PHM) core competencies were published. In response, our hospital medicine section and simulation program assessed and implemented simulation-based training to improve competency.
Objective: Our primary aims were to 1) determine specific knowledge, skill and competency needs in alignment with pediatric hospitalist scope of practice, then use results to design a simulation-based curriculum and 2) implement and evaluate the impact of this curriculum. Secondary aims included describing feasibility and learner satisfaction regarding simulation as a faculty development tool.
Design/Methods: Baseline and post-training surveys were administered to 49 physicians, providing self-ratings from Novice to Expert on published PHM competencies. We averaged participant responses on individual questions into specific domain scores, bundled according to learning content needs. Six targeted simulation sessions were developed, piloted and implemented. Hospitalist faculty participated in simulation at regular intervals over the study period. The change for each domain was assessed with a Sign-Rank test. Each participant was deemed competent in a domain if their mean score was three or greater. The change in competency status was determined using McNemar’s test. We determined if the change in score for each domain was different across years of experience or the number of sessions attended using Kruskal–Wallis tests.
Results: Baseline survey response rate was 98% with 85% completing the post-training assessment. The median number of years of experience as an attending was 4 [IQR: 1-9].
Areas with the lowest self-reported competency on the baseline assessment included medically complex care, code cart, vascular access & emergency medications, advanced airway management, and team communication. Post curriculum scores improved significantly for 5 of 9 domains and percent competent in one domain. Mean scores increased to three or greater in all domains reaching the designated self-assessment competency threshold. Change in scores was not associated with years of experience or increased session attendance. Overall, participants rated the educational sessions “good” or “excellent” at a rate of 98%.
Conclusions: Results from a baseline assessment were instrumental in designing a simulation-based faculty education curriculum. Post-training analysis revealed gains in multiple domains and identified future opportunities for targeted intervention to address persistent competency gaps. Hospitalists reported participation in simulation sessions positively impacted patient care and team communication. As new subspecialists, pediatric hospitalists across the country may find value in a similar process to provide novel faculty education.
-

Development Of Whole-Genome CRISPR-CAS9 Screens To Discover Novel Immunotherapy Targets In Pediatric Leukaemia
Jacqelyn Nemechek, Kealan Schroeder, Jennifer Pace, Bradley C. Stockard, John C. Means, Scott T. Younger, and John M. Perry
Treatment of pediatric leukaemia often involves the use of high doses of anthracyclines, which results in severe side-effects including cardiotoxicity and the development of secondary cancers. Based on previous studies showing that anthracyclines such as doxorubicin (DXR) can target therapy-resistant leukemia stem cells (LSCs) at low, generally non-toxic doses, we repurposed DXR as a targeted inhibitor rather than a broadly cytotoxic chemotherapy. In contrast to typical clinical usage, low-dose DXR treatment reduces expression of multiple immune checkpoint (IC) inhibitors, which exposes LSCs to elimination by cytotoxic T lymphocytes. In the laboratory, anthracyclines can also stimulate immunogenic cell stress/death (ICD). Unlike other forms of cellular death, ICD can induce an anti-cancer immune response, effectively immunizing against cancer recurrence. Unfortunately, this effect is generally not observed in the clinic possibly due to the high-dose, and thus immunosuppressive nature of current treatment regimens. Indeed, our data indicates this is due to fundamentally unique gene expression programs induced by high vs. low doses.
Here, we will test the hypothesis, supported by preliminary data, that low to intermediate DXR exposure reduces IC expression and initiates stress-inducing ICD, respectively. Thus, discovering genes that inhibit or synergize with IC suppression and ICD induction will identify targets that can be activated or inhibited to enhance clinical efficacy of anthracyclines and other ICD-inducers at low concentrations that are not toxic to healthy tissues. Utilizing CRISPR-Cas9 gene editing technology we have developed whole genome screens to construct and validate a chemical-genetic strategy for investigating the effects of differential doses of doxorubicin on leukemia cells for identifying IC suppressors/ICD inducers. Ultimately, this project will reveal novel therapeutic strategies for harnessing the immune system to enhance and potentiate the ICD response of low-dose DXR treatment, thus providing durable, less toxic cures for pediatric cancer.
-

Differences Between Autoantibodies Induced By Sars-Cov-2 Infection And Pfizer-Biontech Sars-Cov-2 Vaccination
Eric S. Geanes, Cas LeMaster, Elizabeth Fraley, Rebecca McLennan, Elin Grundberg, Rangaraj Selvarangan, and Todd Bradley
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection can induce severe disease and lead to hospitalization and/or death in some subpopulations of patients. The underlying mechanisms of disease severity between individuals remain unclear. Recently, autoantibodies have been detected after severe SARS-CoV-2 infection, including anti-idiotypic IgM antibodies targeting ACE2, the receptor for SARS-CoV-2. In this study, we examined autoantibody differences within hospitalized patients with severe SARS-CoV-2 infection, individuals with previous SARS-CoV-2 infection (seropositive), and individuals with no previous exposure to SARS-CoV-2 (seronegative). An autoantibody multiplex panel was run on serum collected from seropositive and seronegative individuals before vaccination and at 7 weeks after two doses of vaccine. Anti-ACE2 antibodies were measured for these samples in addition to serum collected from hospitalized individuals with severe SARS-CoV-2 infection. Severe SARS-CoV-2 infection resulted in elevated anti-ACE2 IgG, IgA, and IgM antibodies compared to all vaccine groups. Seropositive samples resulted in significantly higher anti-ACE2 IgG after vaccination, and significantly higher IgA and IgM antibodies before vaccination compared to seronegative samples. ACE2 inhibition was measured for samples with measurable anti-ACE2 IgG to determine if anti-ACE2 autoantibodies were affecting ACE2 function. The findings of this study elucidate severe SARS-CoV-2 infection results in higher IgG, IgA, and IgM anti-ACE2 antibodies compared to non-hospitalized SARS-CoV-2 infection and SARS-CoV-2 naïve individuals and in turn may provide future novel identifiers for SARS-CoV-2 disease severity.
-

Diffuse Large B-Cell Lymphoma Risk Score Calculator: A Tool To Accurately Predict Survival Risk And Improve Treatment Decisions And Outcomes
Santosh Khanal, Arjun Gampala, Eric S. Geanes, Anne T. Culpepper, Liubomyr Buryi, Catherine A. Jackson, Rebecca McLennan, and Todd Bradley
Diffuse large B-cell lymphoma (DLBCL) is the most common type of non-Hodgkin lymphoma. It is an heterogenous cancer that can have variable responses to therapy and profound differences in survival outcomes. DLBCL is of B- cell origin and was typically treated with a regimen of cyclophosphamide, hydroxydaunorubicin, oncovin and prednisone (CHOP) but the addition of the anti-CD20 monoclonal antibody rituximab (R) significantly improved patient overall-survival (OS). A scoring system has been used to identify risk groups of DLBCL individuals called the International Prognostic Index (IPI) that uses age, lactate dehydrogenase levels, general health status, stage of tumor and number of disease sites to place the patients in 1 of 4 risk groups that correspond with the likelihood of 3-year OS. A revised IPI (R-IPI) using R-CHOP-treated patients was developed that had improved prognostic value at determining risk groups. What this historically used DLBCL scoring system lacks is more individualized data, including molecular information. Limited gene expression studies have been performed on DLBCL, which have successfully classified DLBCL subclasses. Here, we have expanded on previous gene expression studies and have identified genes that are associated with OS in DLBCL using data from the Lymphoma/Leukemia Molecular Profiling Project. Specifically, we have developed a prognostic gene signature consisting of 33 genes that, when transformed into a risk score, can stratify individuals into high or low risk groups that have significantly different OS. The prognostic gene signature was associated with OS in multiple clinical studies, and when used in conjunction with DLBCL molecular subtype and R-IPI score predicted OS with more accurately. Recently, we have developed a web based DLBCL Risk Score Calculator. This calculator combines our prognostic gene signature and the current R-IPI risk scoring system to generate risk scores and predict survival probabilities by year. Next, we will challenge our DLBCL Risk Score Calculator by performing RNA sequencing on DLBCL samples with documented pathology and progress reports. After validation, our DLBCL Risk Score Calculator will more accurately identify patients that will do well on standard care, and alert clinicians to patients that would benefit from experimental therapeutic approaches or more frequent clinical monitoring following treatment.
-

Essential Overlapping Functions Of Crk And Crkl In Glioblastoma And Diffuse Intrinsic Pontine Glioma Cells
Neka Large and Taeju Park
Background: The expression levels of CT10 regulator of kinase (Crk) and Crk-like (CrkL) are elevated in many human cancers, including glioblastoma (GBM) and diffuse intrinsic pontine glioma (DIPG). GBM and DIPG are both highly aggressive brain tumors derived from glial cells. Elevation of Crk and CrkL contributes to poor prognosis, and they have been proposed as therapeutic targets for GBM. We recently demonstrated that Crk and CrkL play essential overlapping roles in GBM cell migration. Here we have investigated if Crk and CrkL play similar roles in GBM and DIPG cells.
Methods: We induced gene knockdown of Crk, CrkL, or both in vitro in a human GBM cell line, U-118MG, and a human DIPG cell line, SF8628 by electroporating with small interfering RNAs (siRNAs). Then we determined the respective, quantitative contributions of Crk and CrkL to cellular phenotypes. Impedance-based, real-time measurements of tumor cell adhesion, migration, and invasion were performed using the xCELLigence Real-Time Cell Analyzer (Agilent).
Results: The combined use of specific and potent Crk and CrkL siRNAs induced effective knockdown of CrkII, CrkI, and CrkL in GBM and DIPG cells. Crk knockdown did not affect cell morphology or proliferation in both GBM and DIPG cells. On the other hand, CrkL knockdown caused shrinkage of cells and inhibition of cell migration and adhesion in both cell lines. In both GBM and DIPG cells, Crk/CrkL double knockdown resulted in more pronounced morphological alterations and robust inhibition of proliferation and adhesion. Furthermore, Crk/CrkL double knockdown completely blocked cell migration and invasion in both cell lines.
Conclusion/Significances: These results demonstrate both the predominant role of CrkL and the essential overlapping functions of Crk and CrkL in GBM and DIPG cells. Our study indicates that migration and invasion of GBM and DIPG cells depends entirely on Crk and CrkL. Our results suggest that inhibition of Crk and CrkL activity may suppress invasion of glioma into healthy brain tissues. Impedance-based, real-time measurement of glioma cell migration represents a robust assay for monitoring Crk and CrkL activities.
Support: Tom Keaveny Endowed Fund for Pediatric Cancer Research (to TP), Masonic Cancer Alliance Partners Advisory Board grants from Children’s Mercy Hospital (CMH) and the University of Kansas Cancer Center (KUCC) (to TP), and Natalie’s A.R.T. Foundation (to TP).
-

Establishing The Role Of Inflammatory Markers In The Diagnosis And Treatment Of Acute Hand Infections In The Pediatric Population
John Schutz, Morgan Williams, Sarah E. Sibbel, and Micah K. Sinclair
Hypothesis: The purpose of this study was to determine the utility of inflammatory markers in diagnosis and treatment of hand and wrist infections in the pediatric and adolescent population. It was hypothesized that there is a difference of inflammatory marker levels between superficial and deep hand/wrist infections at presentation and throughout the course of treatment.
Methods: This is a multicenter, retrospective cohort study included patients age 0-18 who received treatment for an acute hand or wrist infection between 2009 - 2020. Sites included Children’s Hospital Colorado and Children’s Mercy Hospital. Data collected included demographics, diagnosis, inflammatory markers, culture results, antibiotic treatment, and surgical treatment. Infections were categorized as Deep (Osteomyelitis, Tenosynovitis, Abscess) and Superficial (Paronychia, Felon, Cellulitis). Exclusion criteria included: patients >18 y/o, chronic infection, open fractures, absence of inflammatory markers. Statistically, a t-test was used to compare inflammatory markers between deep and superficial infections. Patients who did and did not receive pre-treatment antibiotics were compared separately. Logistic regression models were used to evaluate the association of specific diagnoses with inflammatory markers and/or course of treatment.
Results: 129 patients met inclusion criteria. Deep hand infections (osteomyelitis, tendonitis, and abscesses) were significantly (p=0.0399) associated with a higher ESR (24.8; SD=25.7) than superficial infections (paronychia, felon, cellulitis) (14.5; SD=10.1). CRP and WBC were not significantly different between deep and superficial infections. No significant associations were found between lab markers and course of treatment (operative vs bedside vs oral antibiotics.) Pretreatment with antibiotics at an outside hospital prior to presentation for definitive management was not found to be significantly associated with changes in lab markers.
Conclusions: An elevated ESR is the inflammatory blood marker most predictive of a deep as opposed to superficial hand infections. Inflammatory markers were not significantly different between patients who received pre-treatment with antibiotics and those who did not. Clinicians may use ESR levels to evaluate severity of pediatric hand and wrist infections but should defer to clinical judgement for course of treatment.
-

Feasibility Trial Of Fresh Produce Delivery To Families In Home Visiting Programs
Laura Plencner, Aliyah Hoffmann, Jean Raphael, and Jeffrey D. Colvin
Background: Over 13 million children are food insecure, which is associated with poorer child physical and mental health. Home delivery of produce may improve food security of low-income families. This study assessed feasibility and acceptability of leveraging a home visiting program to directly provide food to families with young children.
Objective: We completed an 8-week prospective feasibility trial of direct food provision using produce from our hospital’s community garden and regional food bank using mixed methods evaluation.
Methods: Twenty-five low-income families participating in an infant home visiting program were enrolled. Produce was harvested from the garden, combined with free food bank produce, delivered to home visitor program office weekly, and then delivered to the family’s home by home visitor. Parents completed surveys to evaluate program satisfaction using Likert scales. Results were analyzed with descriptive statistics. Semi-structured interviews were conducted with 8 participants in English or Spanish. Transcripts were coded using deductive and inductive methods, and thematic analysis completed.
Results: Overall participating families were large and diverse in race, ethnicity, and language. In total 286 bags (1900 lb) of produce were delivered (average weight of 6.8lb/bag; average 6 types of produce/bag). Over half (64%) of participants completed the survey. A majority of participants rated liking the program “very much” (94%) and they would recommend it to another family (100%). Participants reported higher intake of fruits and vegetables compared to before the program (50% “a lot more”; 44% “a little more”) and 94% tried a new food. The program cost $48.80/family for materials (i.e., bags, coolers) and delivery. Thematic analysis of interviews identified (a) food variety and delivery by a familiar person as important, (b) the need for cooking instructions/recipes for the new foods that participants tried, and (c) the positive program impact on the family food purchasing, diet, and budget.
Conclusions: Direct food provision to families enrolled in a home visiting program was acceptable to families and led to increased fruit and vegetable intake and exposure to new foods. This supports a larger trial with a comparison group to evaluate the effectiveness of improving food security and the fruit and vegetable consumption. Partnerships between healthcare institutions and community organizations serving families with young children may make initiatives to address food insecurity and the consumption of fruits and vegetables more effective and feasible.
-

Feeding And Swallowing Disorders In Children With 22q11.2 Deletion Syndrome
Jana Ghulmiyyah, Meghan Tracy, and Jill M. Arganbright
Introduction: 22q11.2 deletion syndrome (22qDS) is the most common chromosomal microdeletion syndromes. The incidence in the literature ranges between 1:1000-1:3000 livebirths. 1,2 These patients present with a wide array of symptoms including, but not limited to, cardiac anomalies, immunodeficiency, velopharyngeal insufficiency, hypoparathyroidism and developmental delay. Feeding difficulties are commonly reported in this patient population however little is known about the pathogenesis, progression over time, and treatment strategies. The goal of this study is to better understand the incidence of feeding difficulties, work-up and management strategies for dysphagia, and outcomes over time for pediatric patients with 22qDS.
Methods: After approval from the IRB, a retrospective chart review was performed for 166 consecutive patients enrolled in the CMH 22q team repository. The charts were reviewed for genetic diagnosis, evidence of feeding difficulties, recurrent aspiration, failure to thrive and dysphagia. We reviewed all patients with oral or pharyngeal dysphagia, aspirations, failure to thrive due to feeding intolerance or aversive feeding patterns. The need for alternative feeding methods such as nasogastric tube feeding or gastrostomy tube feeding were noted. Patients who underwent video fluoroscopic swallow studies (VFSS) were identified and the findings recorded. Patients who underwent flexible and surgical laryngoscopies as well as injection laryngoplasties were recorded.
Results: One hundred and sixty-six patient charts were reviewed. Sixty-five patients (39%) had reported feeding concerns and had been evaluated by a therapist. Structural abnormalities were relatively common with 11% having laryngomalacia and 7% with laryngeal cleft. Thirty-nine patients (28%) underwent a total of 65 VFSS; 13 patients had more than one VFSS. Results of VFSS showed 72.3% had oral dysphagia, 78.5% had pharyngeal dysphagia, and 56.9% showed penetrations into the larynx. Of the 13 with repeat studies and oral dysphagia, 7 patients had no change in their dysphagia, 3 patients had improvement, and 2 patients had worsening. Four percent of patients had reported failure to thrive, and 23% had history of a gastrostomy tube.
Conclusion: Feeding difficulties were commonly reported in our large cohort of patients with 22qDS. It was frequent for patients to be evaluated by a feeding therapist and to undergo formal swallow study. Gastrostomy tube was required in nearly one quarter of patients. Providers caring for patients with 22q should be aware of the potential for feeding difficulties to ensure timely diagnosis and treatment. Future studies are needed to better characterize dysphagia outcomes over time for patients with 22qDS.
-

Genetically Engineered Mouse Models (GEMM) Core At CMRI
Laramie Pence and Jay L. Vivian
The Genetically Engineered Mouse Models (GEMM) core is a CMRI resource created to support investigators in the design, generation, and analysis of novel genetically modified mouse strains in the new state-of-the art vivarium at Children’s Mercy Kansas City. The development of new animal models will provide CMRI researchers an unprecedented tool to investigate the etiology and treatment of pediatric disease. The GEMM core staff have comprehensive expertise in both molecular biology and methods for genetic manipulation of the mouse genome, and the facility is outfitted with the necessary equipment to apply state-of-the-art technologies to our efforts. The GEMM core expertise includes the development, validation, and use of CRISR reagents for efficient genome editing methods in the mouse. In addition to novel model generation the GEMM core offers a host of other support services: cryopreservation of sperm and embryos to protect and archive important strains and storage of these samples in the Children’s Research Institute Biorepository (CRIB), colony maintenance and support for difficult breeding colonies, and importation of mice from outside facilities via in vitro fertilization and rederivation. The GEMM core also supports the design and implementation of an array of genotyping methods, including Transnetyx genotyping services, to maintain the correct allele representation within colonies. These supporting services round out the core's ability to meet the needs of CMRI researchers and to achieve the goal of creating animal models that will advance research in pediatric medicine.
The GEMM core continues to employ and develop cutting edge technology to generate and characterize custom mouse models to address the specific research needs of CMRI investigators. Recently the core staff have developed a genotyping approach that uses Next Generation Sequencing to identify the full gamut of alleles present in CRISPR-edited founder animals. This procedure streamlines what is sometimes a challenging genotyping task and provides a reliable means to select useful founders.
-
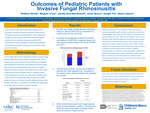
Outcomes Of Pediatric Patients With Invasive Fungal Rhinosinusitis
Madhavi Murali, Meghan Tracy, Janelle R. Noel-Macdonnell, Jason R. Brown, Dwight Yin, and Daniel R. Jensen
Introduction: Invasive fungal rhinosinusitis (IFRS) often manifests in immunocompromised individuals and is challenging to manage. This study sets out to identify outcomes of pediatric patients who have undergone biopsy for suspected IFRS relative to a comparable general population.
Methods: This is a single-site three arm retrospective review of patients diagnosed with suspected IFRS and control patients between January 1, 1995 and April 1, 2019. This review analyzed patients who have received a diagnosis of ALL, AML, NHL, aplastic anemia, or who received an allogeneic BMT during the study period. Qualifying patients aged 21 years old and younger were assigned into one of three groups within the study: an IFRS positive biopsy group, an IFRS negative biopsy group, or a comparable general population group. Patients who had undergone endoscopic surgery due to suspicion of IFRS were included in one of the two IFRS groups. A total of 804 patients were included in this study. Data collected for this study included results of biopsies if conducted, cause of death in patients who received biopsies, and mortality of all patients.
Results: The presence of a positive biopsy for IFRS did not meaningfully affect the mortality rate of pediatric patients relative to those who underwent a biopsy that was negative for IFRS. However, pediatric patients who underwent a biopsy for IFRS—regardless of the outcome of the biopsy—had a higher mortality rate than the comparable general population of pediatric patients (p < 0.05).
Conclusions: Patients who undergo biopsy for suspected IFRS are found to have a higher mortality rate than those of a comparable general population, regardless of the outcome of the biopsy. Additionally, the outcomes of pediatric patients with a positive biopsy for IFRS in this study appeared to better than those in adult counterpart studies. Further studies are being conducted to establish criteria for biopsy in suspected IFRS, which can possibly predict patient mortality and guide clinical decision making.
-

Pediatric COVID-19 Involving Complicated Sinusitis With Intracranial Extension And Lemierre’s Syndrome: A Case Report
Rohit Nallani, Srivats Narayanan, Meghan Tracy, and Jill M. Arganbright
Introduction: Pediatric COVID-19 has been associated with various complications including chronic respiratory disease and multisystem inflammatory syndrome (MIS-C). Otolaryngologic symptoms are common and include sore throat, nasal congestion, and taste/smell disturbances; few cases of complicated sinusitis have been reported. We present a patient with recent COVID-19 who developed complicated sinusitis with intracranial extension and Lemierre’s syndrome.
Case Description: A 16-year-old female presented to the Emergency department with history of COVID-19 diagnosis 17 days prior. She reported worsening symptoms including headache, visual changes, and neck stiffness. Initial concerns for MIS-C prompted admission to the PICU. Exam showed left proptosis, Cranial nerve VI palsy, and limited neck range of motion. She was febrile to 104°F, hypotensive, with elevated WBC 12.7 and CRP 25. MRI brain revealed meningitis, bilateral cavernous sinus thrombosis, and a 3 x 2 x 3 cm sellar/clival abscess. A CT sinus showed severe sinus disease of bilateral sphenoid sinuses. CT neck showed thrombosis of bilateral internal jugular veins consistent with Lemierre’s syndrome. Patient underwent endoscopic sinus surgery including bilateral sphenoidotomies. Small bony dehiscence of the posterior sphenoid wall was identified. Sinus cultures grew Prevotella melaninogenica, Cutibacterium acnes, Staph epidermidis, and MSSA. Blood cultures grew Fusobacterium necrophorum. She was treated with multiple IV antibiotics. Anticoagulation was initiated after surgical intervention. Repeat MRI on postoperative day 20 showed improvement of sinus disease, cavernous sinus thrombosis, and intracranial abscess. Patients’ symptoms slowly improved, and she was discharged home on hospital day 21.
Discussion: This is the first pediatric report describing complicated sinusitis with an intracranial abscess, bilateral cavernous sinus thrombosis, meningitis, and Lemierre’s syndrome following COVID-19. Early surgical intervention, IV antibiotics, and anticoagulation were important for her recovery. Providers caring for patients with COVID-19 should keep complicated sinusitis and Lemierre’s in their differential. Future studies assessing the impact of COVID-19 on the pediatric sinonasal cavity are needed.
-

Pilot Study Of Mhealth Adherence By Parents To A Pediatric Developmental Application For Infants After Neonatal Cardiac Surgery
Amanda Manderfeld, Jennifer A. Marshall, Elizabeth J. Willen, Jami Gross-Toalson, Amy Ricketts, Melissa D. Elliott, Nickey Crail, and Lori Erickson
INTRODUCTION: The use of mHealth applications is widespread in adult care and been used less in pediatric care due to the unique challenges of pediatric interventions, especially for children with congenital heart disease (CHD)1. High incidence of mobile phone ownership provides low-cost, broad reach intervention for developmental support for pediatric populations2-3. Infants with CHD are at a high risk for experiencing multiple developmental delays4. Study purpose is to evaluate mHealth adherence and acceptance of a developmental application, Babysparks©, by parents of infants with CHD.
METHODS: A single site, cross sectional, pilot study, with a pre/post-test design was used to evaluate the mHealth adherence at parental self-imposed rate over 6 months after pediatric CHD surgery for children < 18 months.
RESULTS: Of 101 potentials, 66 parents enrolled with 83.1% (n=54) successfully initiating the app link. Utilization of the developmental videos was found in 29 parents (43.9%). No differences in SES were noted, but a higher rate of adherence for parents of children with feeding tubes v. PO feed solely (p=.021) with only 37.9% (n=25/66) PO feed solely. 87.3% of parents reported daily mobile phone use and a low rate of utilization of therapies outside the hospital was noted at 44.6%. Table 1 is rate of adherence. Implementation was highest with gross motor (89.6%, n=26/29) and speech (75.9%, n=22/29). At study exit, 87.2% (n=34/39) of parents reported the app was easy to use and 100% (n=39/39) agreed that regular use of this app would help other children with CHD.
DISCUSSION: Adherence initiation of the mHealth app was high but implementation of the videos was low at 43.9%, likely due to self-management factors with additional stress of complex care regimens including pediatric feeding tubes. Developmental milestones were more frequently reached when the videos were accessed. A key area of future research is two-way communication with the CHD developmental team utilizing the mHealth dashboard and implementation rates of use with parents.
-

Providing Antiicipatory Guidance For Children With Medical Complexity And Gastrostomy Tubes: Feasibility And Impact Of An Online Curriculum For Residents
Emily J. Goodwin, Robert Riss, Elena Huang, Evan Weber, Elizabeth Rhyne, and Jeffrey D. Colvin
Anticipatory guidance (AG) is essential for all children, especially children with medical complexity (CMC). CMC often rely on medical devices, most commonly gastrostomy tubes, and benefit from proactive AG. However, few curricula have been developed to train residents in providing applicable AG for CMC.
Our objective was to examine the feasibility and impact of an asynchronous online curriculum for residents on providing AG for children with gastrostomy (GT) or gastrojejunostomy (GJ) tubes. Informed by the results of a needs assessment at a large free-standing children’s hospital, we designed and implemented an online asynchronous curriculum for residents using Kolb’s experiential framework.
The four-week course included four modules instructing residents on principles of AG in CMC, GT and GJ basics and troubleshooting. We also included downloadable toolkits with sample smart phrases for documenting exam findings and AG. We assessed knowledge, attitudes, and behaviors related to the curriculum via pre- and post-tests, an anonymous course evaluation, and optional semi-structured interviews. Pre-test and post-test answers were compared using McNemar’s Test, using a test score of 70% to represent adequate knowledge. We used descriptive statistics to assess the results of the course evaluation and thematic content analysis to identify themes from semi-structured interviews.
A total of 102 residents participated in the course; 91 (89.2%) completed the course evaluation and 75 (73.5%) consented to the use of their data in this study (Table 1). The percentage of residents scoring ≥70% on the post-test was significantly higher than on the pre-test (4.7% pre- vs. 96.9% post-, p < 0.001) (Table 2). Residents also reported improved comfort in all assessed activities (comfortable: 34.7%-63.9% pre- vs. 100.0% post-, p < 0.001) (Table 2). The majority agreed or strongly agreed that the course was relevant (86.9%), course objectives were met (88.1%), and time to complete it was reasonable (73.8%). Themes from interviews of 8 residents bolstered these findings: residents perceive barriers in giving AG to CMC and residents learned valuable skills from the curriculum (Table 3).
In conclusion, an online asynchronous curriculum to teach residents how to provide AG for CMC with GT or GJs was feasible, effective, and well received. Future directions include assessing resident documentation of AG in visits with CMC related to GTs to further assess behavior change and the application of knowledge and skills acquired from the curriculum.
-

Rate Of Depression Among Primary Caregivers Of Children With Tracheostomies
Madhavi Murali, Alexandra Arambula, Meghan Tracy, Ashley Sherman, Cameron J. Farsar, and Jason R. Brown
Introduction: Caring for a child with a tracheostomy carries numerous financial, physical, and emotional challenges. Literature has shown that these caregivers experience burden that correlates with their child’s illness severity and their own mental health status. Caregivers of technology-dependent and chronically ill children have been found to have higher rates of depression, but similar findings have not been reported for pediatric tracheostomy caregivers. Thus, the objective of this study was to assess rates of depression among primary caregivers of children with tracheostomies.
Methods: A database of children (ages 0-18) with tracheostomies at a tertiary pediatric hospital was screened to identify patients’ primary caregivers. Exclusion criteria included state custody/foster care, lack of follow-up within the past 2 years, caregiver age < 18, and a caregiver-reported history of depression. Eligible caregivers were contacted over a 3-month period; participants completed a demographic form and the Beck Depression Inventory-II (BDI-II). Mental health resources were offered if BDI-II scores indicated any level of depression and caregivers agreed to receiving resources. Basic patient health data were also collected.
Results: Of 207 children, 129 had caregivers eligible for participation. Forty-five caregivers (35% response rate) participated; 6 had prior diagnoses of depression, leaving 39 caregivers for analysis. The majority of caregivers were female (95%), aged 25-44 (77%), white/Caucasian (77%), married (77%), and receiving some Medicaid benefits (97%). Of 38 caregivers who completed the BDI-II, 29% (11) met criteria for at least mild clinical depression, with 7/11 meeting criteria for moderate or severe depression. Only 1 of these 11 caregivers agreed to receive mental health resources. There was no significant association between BDI-II scores and patient comorbidities or caregiver insurance, age, gender, or race.
Conclusion: Nearly 1/3 of our pediatric tracheostomy caregivers had some degree of clinical depression based on BDI-II scores. To our knowledge, this is the first study assessing rates of depression within this caregiver cohort. Based on our findings, these caregivers’ psychosocial needs may benefit from further exploration to enhance available supportive resources.
-
Risk Factors For Failure Of Cast Immobilization In Pediatric Scaphoid Fracture Presenting Greater Than 28 Days After Injury
Joshua Lackey, Paige Pearson, Brian Lee, and Micah K. Sinclair
Hypothesis - In pediatric patients who sustain a scaphoid fracture, cast immobilization will result in successful union at a lower rate in delayed presentation ( > 28 days following injury) of displaced fractures with cystic change than acute, nondisplaced fractures without cystic change after 12 weeks of casting.
Methods - A retrospective analysis of 255 scaphoid fractures treated at a single pediatric hospital between 2010-2020 was performed to characterize: demographic factors, fracture characteristics, amount of cystic change, treatment method, and rate of healing. The primary outcome measure was the rate of healing of scaphoid fractures presenting > 28 days from injury with cast immobilization and compared with those treated surgically. Demographic factors and fracture characteristics were compared using Fisher's exact tests.
Results - Patients presenting in a delayed fashion were more likely male (84.8%, p = 0.02), injured playing sports (63%, p < 0.0001), football players (41.3%, p < 0.0001), and had closed physes (41.3%, p < 0.0001). The fracture characteristics included an increased incidence of a transverse fracture pattern (80.4%, p = 0.037), proximal pole fracture (26.1 %, p < 0.0001), > 1 mm of cystic change (80.4%, p < 0.0001), and > 1 mm of fracture displacement (62.2%, p < 0.0001). Of patients presenting in a delayed fashion, 41.3% were treated with casting alone with a 78.9% union rate compared to 96.1% of acute fractures treated with casting resulting in a 95.5% union rate. The average duration of casting required for healing in the delayed presenting fractures was 63 days (range 53-98). There were no significant demographic differences between the patients with chronic scaphoid fractures treated with casting or surgery initially. However patients treated with casting were less likely to have cystic change > 1 mm (42.1%, p = 0.002), fracture displacement (73.7%, p = 0.0001) or fracture comminution (5.3%, p = 0.031.)
Summary points -
-
Cast immobilization for scaphoid fractures who present > 28 days following injury results in successful union in patients with minimal displacement, < 1 mm cystic change, and no fracture comminution or humpback deformity. These indications for casting mirror the acutely presenting group.
-
Both acute and delayed groups treated with casting healed in an equivalent amount of time.
-
Sports participation, specifically football participation, is a risk factor for delay of presentation of pediatric scaphoid fractures.
-
Delayed presentation of a scaphoid fracture is not independently an indication for surgery in the pediatric and adolescent population.
-
-
Single-Cell Genomic Data Reveals Heterogeneity In Infant Acute Lymphoblastic Leukemia
Irina Pushel, Midhat Farooqi, Sidharth V. Ramesh, Byunggil Yoo, Daniel A. Louiselle, Patrick A. Brown, and Erin M. Guest
Infant acute lymphoblastic leukemia (ALL) is an especially aggressive form of leukemia, particularly among patients with a rearrangement in the KMT2A gene (KMT2A-r). Approximately two-thirds of infants with KMT2A-r ALL relapse within a year of initial diagnosis, with relapsed disease particularly resistant to treatment and associated with high mortality. The ability to better predict which patients are likely to relapse, especially relative to current residual disease detection methods like flow cytometry, would greatly improve treatment selection and patient outcome. In this study, we set out to identify novel prognostic markers in patient data at diagnosis. We utilized 10X Genomics single-cell RNA sequencing (scRNAseq) of bone marrow or peripheral blood samples with leukemic cells at diagnosis and compared gene expression between infants with KMT2A-r ALL who later went on to relapse (n = 19) versus those who did not (n = 6). Differential expression analysis identified novel cancer-linked genes associated with future relapse (n = 484), including NR5A2, TP53BP2, and BCL2L11, or lack of future relapse (n = 461), including CSMD1 and SCAI. Taking advantage of the single-cell resolution of our dataset, we also applied a recently published tool for assigning scores predicting resistance or sensitivity to treatment for individual cells. Consistent with the literature, patients in our dataset who went on to relapse had a significantly higher proportion of treatment-resistant cells at diagnosis than those who did not go on to relapse, further suggesting the prognostic value of this metric. Overall, this study leveraged scRNAseq data to identify multiple tools that can be used to predict relapse risk in infants with KMT2A-r ALL. These findings should enable better patient risk stratification and therapy selection at diagnosis for infants with this aggressive disease and may also lead to the development of novel individualized treatments in the future.
-

Socioeconomic Status And Household Material Hardship In Children With Medical Complexity
Margaret Wright, Isabella Zaniletti, Rupal Gupta, Ingrid Larson, Courtney Winterer, and Jeffrey D. Colvin
BACKGROUND:
Children with medical complexity (CMC) have complex chronic conditions and increased acute care utilization, impacting health-related quality of life (HRQOL). Families of CMC are more likely to have low income and food insecurity. Other measures of socioeconomic status (SES) and household material hardship (HMH) have not been examined in families of CMC, nor has the relationship of SES and HMH with acute care utilization and HRQOL.
OBJECTIVES:
Examine SES and HMH in CMC and its relationship with HRQOL and acute care utilization. Examine predictors of family financial difficulty related to the child’s health conditions.
DESIGN/METHODS:
250 parents of CMC completed surveys containing items related to SES, HMH, and HRQOL. Predictors were SES and HMH. SES was measured as income, wealth (car/home ownership), and parental education. HMH was measured as food, housing, or utilities insecurity. Outcomes were child HRQOL, acute care utilization, and family financial difficulty. HRQOL was measured using validated CP-QOL and Functional Status II instruments; total HRQOL was converted into a Z score. Acute care utilization was measured as annual ED visits, hospitalizations, and costs. Utilization data were collected from hospital administrative data. We examined bivariate associations with the X2 test. For bivariate associations with p<0.10, we performed generalized linear and logistic models, adjusting for demographic and clinical characteristics. We performed a classification and regression tree (CART) analysis.
RESULTS:
Table 1 describes the study population characteristics and association with outcomes. 60.4% of families reported income below the FPL, and 69% completed education less than a college degree. 40% reported at least one HMH. SES and HMH were not associated with HRQOL. Education was associated with acute care utilization. HMH was not associated with utilization. In adjusted analyses, education was not associated with costs, but was associated with ED visits: parents with advanced degrees had 8 more ED visits/year than parents with high school degrees (7.9 [95%CI: 4.3, 14.7], p<0.01). HMH was associated with family financial problems, with odds of financial problems increasing with number of hardships (6.9 [95%CI: 2.3, 20.2], p<0.001). By variance importance factor and cross-validation of CART analysis, HMH remained a strong predictor of family financial difficulty.
CONCLUSION(S):
HMH were common in this study population. Higher parental education was associated with more ED visits, but there was no association between other facets of SES or HMH and HRQOL or acute care utilization. HMH was associated with increased odds of family financial difficulties related to the child’s health conditions, regardless of SES.
-
T Cell Populations And Response To Chemotherapy In Human Leukemia
Sara McElroy, Fang Tao, John Szarejko, and John M. Perry
Background
One important prognostic indicator in pediatric leukemia is minimal residual disease (MRD) detected at the end of induction chemotherapy. Detecting any level of MRD in the bone marrow (BM) at the end of induction (MRD+) is associated with increased risk of relapse and poorer overall survival compared to having no MRD detected (MRD-). Discovering differences between these patients, specifically in T cell subsets such as memory T cells and T memory stem cells (Tscm), could lead to new targets for cancer therapy and improvement in treatment for higher risk disease.
Objective
To determine potential differences in the frequency of T cell populations in human leukemia in patients with MRD+ versus MRD- disease after induction chemotherapy.
Design/Method
Samples were from 8 patients with premature B cell acute lymphoblastic leukemia (pre-B ALL) from BM. Timepoints were diagnosis and day 29 (D29) of induction chemotherapy. 4 patients were MRD+ after induction and 4 patients were MRD-. Flow cytometric analysis of cytotoxic memory T cell populations was performed and analyzed using descriptive statistics and the t-test.
Results
For all patients, both MRD+ and MRD-, the mean live cell percentages were not different between diagnosis and D29 (76.9% vs 85.1%, p=0.111). CD3+, CD4+, and CD8+ T cells were all higher at D29 (CD3+- 2.1% vs 6.5%, p=0.011; CD4+- 1.0% vs 2.7%, p=0.044; CD8+-0.8% vs 2.7%, p=0.018). Naïve T cells increased from diagnosis to D29 (0.4% vs 3.4%, p=0.009). Tscm were also elevated at D29 (0.01% vs 0.08%, p=0.042). When the patients were subgrouped based on MRD status, similar differences were seen in the MRD- group between diagnosis and D29 (CD3+- 2.2% vs 7.8%, p=0.039; CD4+- 0.8% vs 4.0%, p=0.035; CD8+- 1.1% vs 3.3%, p=0.073; Naïve- 0.4% vs 3.8%, p=0.039; Tscm- 0.02% vs 0.1%, p=0.037). In the MRD+ subgroup, none of the previously described differences were detected (CD3+- 2.0% vs 5.1%, p=0.197; CD4+- 1.1% vs 1.4%, p=0.644; CD8+- 0.6% vs 2.17%, p=0.175; Naïve- 0.5% vs 2.95%, p=0.173; Tscm- .004% vs 0.02%, p=0.355).
Conclusion
Recovery of immune function is anticipated after induction chemotherapy for pre-B ALL. Our data demonstrate the expected increase in T cell subsets in patients with MRD- BM at D29 but not in patients with MRD+ BM. The discovery of poorer immunological recovery in MRD+ patients requires additional study to determine what makes MRD+ disease different. This could introduce new immunotherapy targets in human leukemia.
-

The Cellular Dynamics Of Early And Transitional Human Breast Milk
Cas LeMaster, Stephen Pierce, Eric S. Geanes, Santosh Khanal, Staci Elliott, Allison Scott, Daniel A. Louiselle, Rebecca McLennan, William E. Truog, Devika Maulik, Tamorah Lewis, Tomi Pastinen, and Todd Bradley
Breast milk (BM) is a complex fluid containing factors essential for infant nutrition and immunity. Breastfeeding has been shown to be protective against infections and other immune-mediated diseases during the lacation period and beyond in later childhood. This suggests that BM also imprints the neonatal immune system and influences long-term health. BM also contains populations of maternal-derived cells. Which factors in BM that are important for neonatal health and how they change during lactation have not been well-defined. In this study, we used a single-cell transcriptomic approach to identify and define cell types of early and transitional milk. We collected BM samples from mothers of infants 2-7 days (early milk) and 8-16 days (transitional milk) after delivery. We applied single-cell RNA sequencing on over 154,000 BM-derived cells. We identified 25 transcripionally distinct populations of cells in the BM. As expected, the most abundant cells in BM were mammary epithelial cells and macrophages. Monocytes, T cells, dendritic cells, and neutrophils were also present and had a higher frequency in week 2, suggesting that some immune cells may remain abundant in the early days of lactation and slowly decline as milk matures. We also detected a small number of stem and progenitor, natural killer and B cells in the BM at a higher frequency in week 1. This work provides an atlas of the cellular component in human milk at two timepoints of lactation. In addition to cell identity and frequencies, we have also uncovered unique molecular pathways that are activated in BM cells. This work will lay the foundation for future studies of how these cells influence neonatal health.
-
The Sars-Cov-2 E Protein Induces Pro-Inflammatory Tlr Signaling, Lung Injury And Alveolar Remodeling In The Neonatal Lung
Heather Menden, Wei Yu, Sherry M. Mabry, Aparna Venkatraman, and Venkatesh Sampath
Background: The delta variant of SARS-CoV-2 is reported to cause severe acute lung injury (ALI) in neonates. Neonates with COVID-19 can exhibit a hyper-inflammatory response with vascular injury. The mechanisms by which SARS-CoV-2 structural proteins induce ALI in neonates is unclear. Emerging data suggest that the envelope (E protein) of the SARS-CoV-2 activates Toll Like Receptor (TLR)-mediated immune hyperactivation and cytokine storm. We tested the hypothesis that SARS-CoV-2 E protein can induce TLR-mediated inflammation and ALI in a neonatal mouse model of ALI we developed.
Objectives: 1) To investigate the pathogenicity of E protein in causing neonatal ALI and alveolar remodeling and, 2) To determine whether E protein induces TLR-dependent cell death and inflammation in human pulmonary microvascular endothelial cells (HPMEC).
Methods: We developed a model of systemic E protein-induced ALI using intraperitoneal injections of 10μg (2mg/kg/dose) in P5 [saccular stage] C57BL6 mice. Lung homogenates were used for quantifying cytokine RNA expression and TLR signaling (immunoblotting) 48h after E protein injections. Bronchoalveolar lavage (BAL) was done on P11 mice 48h after i.p E protein. E protein-induced alveolar remodeling was examined by morphometry on P14 after injecting one dose (P5) or two i.p doses (P5 and P8). Neonatal HPMEC (ScienCell) were treated with 500ng/mL E protein, with or without silencing of TLR2 (siTLR2), and cell lysates were examined for cytokine expression and TLR signaling.
Results: E protein induced lung Cxcl1, iNOS, Il-1β, and Tnfαexpression in a dose-dependent manner at 48h. Activation of TLR signaling was evidenced by phosphorylation of inhibitor of kappa B kinase β (pIKKβ) and the NFKB subunit p65 (Fig.1). BAL showed increased albumin content and neutrophil and lymphocyte infiltration 48h after i.p E protein. E protein-induced alveolar simplification was evidenced by decreased radial alveolar counts on P14. (Fig. 2). E protein dose-dependently induced HPMEC cell death [Fig. 3a], as well as TLR signaling [p-IKKβ], NFKB activation [p-p65], and MAPK signaling [p-p38] in HPMEC. E protein (500ng/ml) induced ICAM1, IL-1β, TNFα, IL6, IL8, and TLR2 expression was suppressed by silencing TLR2 using siRNA. (Fig. 3)
Conclusion: The SARS-CoV-2 E protein induces TLR signaling, ALI and alveolar remodeling in the neonatal lung. Ongoing studies suggest that E protein induces direct EC injury in human lung EC that is TLR2-dependent. This study provides mechanistic insight into neonatal immune activation and lung injury seen in infants with COVID-19.
-

The Sssh’s: Snoo Smart Sleeper Use In Post-Operative Infants With Congenital Heart Disease
Shannon Lysaught, Lori Erickson, Jennifer A. Marshall, and Keith Feldman
BACKGROUND: Children’s Mercy admits approximately 300 patients per year under 6 months of age who require cardiac surgery. Post-operative management of these infants is complex, necessitating soothing interventions to maintain infant reserves necessary for growth and development. Parents cannot always be available and staffing ratios do not always allow for immediate attention to soothe.
TEST ARTICLE: The SNOO Smart Sleeper responds to an infant’s cry with the proven elements of soothing through swaddling, motion, and noise while demonstrating safe infant sleep practices. The prior success of the SNOO in other fragile infant populations (e.g., those with neonatal abstinence syndrome) suggests the possibility for its use in the high-risk congenital heart disease population during the post-operative recovery phase.
OBJECTIVE: To demonstrate the willingness of staff and parents to use the SNOO for post-operative cardiac infants and evaluate the feasibility of collecting a participant’s timestamped data elements representing hemodynamic changes (e.g., heart rate, respiratory rate) and pain medication usage from the cardiorespiratory monitors and electronic medical record (EMR).
HYPOTHESIS: Staff and parents of cardiac infants will be willing to utilize the SNOO during post-operative recovery from cardiac surgery. Clinical data could be aligned with the SNOO sleep log to allow for future investigation of physiologic trends during SNOO usage.
RATIONALE: Post-operative cardiac infants can be difficult to manage on a medical/surgical floor where staffing ratios do not always allow staff to provide immediate soothing measures. The SNOO Smart Sleeper responds to an infant’s cries with movement and white noise, providing immediate soothing until a staff member can intervene.
PROCEDURES: Thirteen potential participants were approached to utilize the SNOO instead of a hospital crib throughout their stay on a medical/surgical unit. Processes to collect and link data elements from participant’s cardiorespiratory monitors and EMR with SNOO sleep logs were developed over a 14-month period.
-

Tonsillectomy In Children With 22q11.2 Deletion Syndrome
Jill M. Arganbright, Meghan Tracy, Srivats Narayanan, and David G. Ingram MD
Introduction: 22q11.2 deletion syndrome (22qDS) is a common genetic disorder with an estimated risk of obstructive airway symptoms in 10-37% of affected children. While tonsillectomy is commonly pursued in an effort to ameliorate airway obstruction this population, there are currently no published studies evaluating tonsillectomy outcomes in children with 22q11DS. Our goal was to investigate the indications, efficacy, and complications of tonsillectomy in a large cohort of patients with 22qDS.
Methods: We performed a retrospective chart review of 168 consecutive patients with 22qDS from the institution’s 22q repository from 1/1/2010-6/1/2021. Data was collected for tonsillectomy indications, length of hospital stay, complications, and pre- and post-op sleep study results.
Results: Thirty-three of the 168 (20%) patients with 22qDS in our sample underwent tonsillectomy. Indications for tonsillectomy included: to facilitate with speech surgery (n=21), sleep disordered breathing/OSA (n=16), dysphagia (n=3), and airway management prior to trach decannulation (n=2). Average length of stay was 1.15 days (range 0-4 days). Six patients had a pre-op sleep study, 10 patients had post-op sleep study, and 3 patients had both a pre- and post-op sleep studies. Of those children who had post-op sleep studies, 3 were normal, 5 had mild OSA, 1 had moderate OSA, and 1 had severe OSA. Three patients presented with post-op tonsil bleeds, of whom 1 required surgical cauterization and 2 recovered with observation alone. In the 8 patients who had post-op calcium monitoring, 4 (50%) had hypocalcemia and endocrine was consulted; 1 patient was treated with oral supplementation, and 3 were observed with repeat labs. One patient experienced postoperative respiratory failure requiring overnight intubation.
Conclusion: Tonsillectomy was a commonly performed procedure in this large cohort of patients with 22qDS. Facilitation of speech surgery and sleep disordered breathing were the most common indications. Most patients spent one night in the hospital prior to discharge. These data highlight the potential need for close post-op calcium and respiratory monitoring. Our data were limited with respect to polysomnographic outcomes, where future studies are still needed to better characterize sleep disordered breathing outcomes following tonsillectomy for patients with 22qDS.
-

Unanticipated PICU Transfers Of Patients Admitted From The Pediatric ED
Allison Adam, Vivek Dubey, Jonathan Rodean, Lisa Carney, Stephen Pfeiffer, Kelli L. Behr, and Shobhit Jain
Objective
This study aims to describe the population of patients admitted from the Emergency Department (ED) who were transferred to the PICU within 24 hours of admission and identify patterns in this patient population. It is part of an ongoing study that aims to identify predictive factors for PICU transfers while accounting for variables like seasonality and staffing.
Design/Methods
This study was conducted at a quaternary children’s hospital with 2 EDs - combined volume of 95,000 annual visits with an 11% admission rate. From chart review starting in July 2020, clinical information was gathered for patients admitted to the inpatient wards from the ED who were then transferred to the PICU within 24 hours. The demographic variables and clinical characteristics among this patient cohort were reviewed by a multidisciplinary team. The length of stay in relation to timing of transfer was also studied.
Results
From July 2020 to December 2021 there were 128 events requiring transfer to the PICU, roughly 1.4% of admissions from the ED over that time. Patients under 2 years of age accounted for 26.4% of all admissions from the ER but 50.8% of all rapid transfers to the PICU were children under 2 years. Respiratory etiology accounted for 69.6% (n=89) of transfers, with combined Rhino/Enterovirus and RSV infection being the largest subgroup (n=47, 43.5%). Most transfers occurred within 12 hours of admission from the ED (n=87, 68%). Early transfers were associated with a shorter total hospital stay - median (IQR) length of stay was 3 days (2, 4) for patients transferred within 6 hours, compared with those between 6-12 hours (4.5 days (3, 8)) and 12-24 hours (5 (3, 10)).
Conclusion(s)
The preliminary data is shared from a local collaborative group comprised of ED, PICU, hospitalists, and transport services. 18 months of data suggest that nearly half of all transfers to the PICU occur in children less than 24 months of age and 69.6% of all unanticipated transfers are due to a respiratory etiology. This requires validation at other institutions while the Rapid/Unplanned PICU Transfer Collaborate at Children’s Mercy continues to identify areas for improvement.
Printing is not supported at the primary Gallery Thumbnail page. Please first navigate to a specific Image before printing.



