These posters have been presented at meetings in Children's Mercy and around the world. They represent research that was done at the time they were created, and may not represent medical knowledge or practice as it exists at the time viewers access these posters.
-

Post-Operative Diagnosis of Anomalous Left Coronary Artery From The Right Pulmonary Artery via Transthoracic Echocardiogram
Lavina Desai, Sanket Shah, Edo Bedzra, and Christopher Mathis
A term infant female was diagnosed with a ventricular septal defect (VSD) and aortic coarctation. Preoperative echocardiography and computed tomography angiography (CTA) showed a normal right coronary artery origin, but inconclusive left coronary artery (LCA) origin. There was a normal flow profile in the LCA by echocardiography. She underwent repair with extended end-to-end anastomosis and VSD closure during which surgical inspection revealed a usual appearing, retro pulmonary path of the LCA towards the left sinus of Valsalva. Postoperative echocardiogram revealed mild global dysfunction but no regional wall motion abnormalities. Repeat echocardiogram revealed severe dysfunction most prominent in the anterolateral and posterolateral segments from base to apex. There was new, bidirectional flow in the LCA and abnormal diastolic flow in the posterior right pulmonary artery (RPA) raising suspicion for anomalous origin of the LCA from the RPA (ALCARPA). Cardiac catheterization confirmed the diagnosis. Echocardiography plays a vital role in detection of ALCARPA. However, the usual clues of flow reversal in the LCA, abnormal diastolic flow in the pulmonary artery and sequelae of left ventricular ischemia vary with age and pulmonary artery pressure. CTA is valuable in diagnosis but may suffer from improper contrast timing and motion artifact. When the LCA originates from the RPA, the origin appears normal due to its proximity to the left sinus of Valsalva, even by visual inspection. Meticulous coronary imaging and clinical suspicion are required for timely detection. Invasive angiography is the gold standard for diagnosis. There are few cases associating ALCARPA with aortic coarctation. Presence of a coarctation and VSD lead to sufficient pulmonary hypertension for antegrade LCA flow which hinders the preoperative diagnosis. This case is unique because the coronary anatomy was interrogated before surgery, but ALCARPA was not demonstrated due to a low index of suspicion for this rare anatomy and associated pulmonary hypertension. This case highlights the diagnostic challenge of this association of defects and reiterates the importance of definitive coronary imaging preoperatively. Persistent myocardial dysfunction following coarctation and VSD repair should prompt careful evaluation for ALCARPA.
-
Rhabdomyolysis As a cause of PTH independent hypocalcemia in a child with acute influenza infection
Samhita Bhattarai and Kelsee Halpin
INTRODUCTION Hypocalcemia is characterized by abnormally low level of calcium in the blood. Normal reference range for calcium for children between 12- 19-year-old is 8.5-10.6 mg/dl . Severe hypocalcemia is considered as serum calcium level of <7 mg>/dl and can present with tetany, seizures, and life-threatening cardiac arrhythmias. Etiology of hypocalcemia varies but hypoparathyroidism, pseudohypoparathyroidism and Vitamin D deficiency are some of the most common causes encountered by pediatrician endocrinologists. Association of rhabdomyolysis with hypocalcemia and elevated PTH is a rare presentation that should be considered, particularly for those children presenting with acute viral illness. We present a rare case of rhabdomyolysis associated with hypocalcemia not related to hypoparathyroidism. CASE A 12-year-old female presented to the emergency department with body ache, decreased oral intake and vomiting. She was found to be influenza positive. Electrolytes showed hypocalcemia (4.8 mg/dl). She subsequently had an undetectable 25-OH vitamin D level (<5 ng>/ml) and elevated iPTH level (609 pg/ml). We discussed the possibility of her etiology of hypocalcemia to be Vitamin D deficiency although her presentation was atypical at an older age with a negative imaging for rickets, hyperphosphatemia (6.0 mg/dl), and normal alkaline phosphatase (334 unit/L). She also did not have any phenotypic features of Albright’s hereditary osteodystrophy and renal function was within normal limits. She was identified to have elevated creatinine kinase (4829 U/L) supporting rhabdomyolysis secondary to acute influenza as a cause of her hypocalcemia. Rhabdomyolysis, a known complication of influenza infection, causes cell membrane destruction which impairs the normal function of Na-K-ATPase channel. This leads to increase in intracellular sodium activating Na/Ca exchanger which in turn causes influx of calcium intracellularly causing hypocalcemia. Additionally, any injury or infection leads to high phosphorus release from cells due to cell lysis. High phosphorus is also caused by reduced oxidative metabolism in muscles impairing phosphate use. This excess of phosphate then combines with calcium and causes calcium-phosphate complex in soft tissues. Hyperphosphatemia also additionally inhibits 1 alpha hydroxylase limiting formation of calcitriol leading to hypocalcemia. CONCLUSION Our patient had severe hypocalcemia due to influenza-related rhabdomyolysis. Rhabdomyolysis is an important consideration as a cause of hypocalcemia in children, especially with acute viral illness. Accordingly, it is also important to obtain serum electrolytes in patients presenting with rhabdomyolysis as hypocalcemia may lead to complications like seizures and cardiac arrhythmia if not appropriately recognized and treated.
-

Children's Mercy: Dedicated to All Children, Everywhere
Heather Steel, Katie Dayani, Julia McBride, Keri Swaggart, and Kim Weir
Children’s Mercy Kansas City was founded in 1897 by sisters Drs. Alice Graham and Katharine Richardson. Their primary objective was to create a hospital where the children of Kansas City and surrounding areas could be treated regardless of their religion, race, or ability to pay. By the early 1920’s segregation became a huddle to accomplishing this dream. To circumvent this problem Dr. Katharine Richardson partnered with Dr. John E. Perry and the staff at Wheatley Provident Hospital, the first private Black hospital in Kansas City, MO, to establish the Mercy Model Ward. This ward provided pediatric care for the Black children in Kansas City and was the first of its kind in the nation. Dr. Richardson was fully committed to providing care to all children, everywhere and this model ward provided the means for her to truly realize her goal.
-

Dental Manifestations and Management of a Pediatric Patient with Hypophosphatasia: Case Report and Literature Review
Dev Patel, Robin Onikul, Amy Burleson, Brenda S Bohaty, Jenna Sparks, and Neena Patel
Hypophosphatasia is a rare autosomal recessive disorder affecting the ALPL gene, which is involved in mineralization of bones and teeth. Given the importance of mineralization on proper tooth development, patients with hypophosphatasia present with numerous dental manifestations and require careful, coordinated care to maintain function and esthetics. This case report details a 9-year-old patient presenting to Children’s Mercy Kansas City Dental Clinic with complex medical history including hypophosphatasia, hypophosphatemic rickets, and developmental delay. The case report will include the patient’s clinical and radiographic presentation and will detail the patient’s treatment history. The presentation will also review the relevant scientific literature regarding hypophosphatasia and the clinical expectations for overall care.
-

Dental Manifestations of a 4-year old Male Patient with Congenital Vitamin D Rickets: Review of the Literature and Report of a Case
Richard Nguyen, Robin Onikul, Brenda S. Bohaty, Neena Patel, Jenna Sparks, and Amy Burleson
Patients that present with Vitamin D-resistant rickets may have abnormal tooth morphology, such as enlarged pulp horns that may extend into the dentino-enamel junction. As a result of this communication, there may be an increased chance of pulpal infection, resulting in spontaneous dental abscesses occurring without evident caries or history of trauma. The purpose of this poster is to report the case of a four-year-old patient who presented to Children’s Mercy Kansas City Dental clinic with chief concern for swelling of the face with unknown causes. The patient’s medical history was significant for congenital Vitamin D-resistant rickets. The poster presents a review of the literature regarding various dental treatment considerations for patients with Vitamin D-resistant Rickets and discusses the dental and medical implications of Vitamin D-resistant Rickets for future care.
-

Differential Diagnosis of a 12-year-old Presenting with a Nodular-Sessile Lesion on the Hard Palate: Review of literature and report of a case.
Meredith Clark, Robin Onikul, Amy Burleson, Brenda S. Bohaty, Jenna Sparks, Neena Patel, and A Naidu
Soft-tissue lesions in children present with a wide range of etiologies, including those related to normal development, underlying systemic illness and/or those associated with benign or malignant tumors1 . In children and adolescents, the most common soft tissue lesions include, aphthae, fibromas, papillomas, pyogenic granulomas and traumatic lesions all of which may present on the hard palate.2 This case report details a 12-year-old female presenting to Children’s Mercy Dental Clinic with a chief complaint of a flesh-colored nodular sessile lesion visualized on the anterior hard palate, directly posterior to teeth #8 and #9. The patient’s medical history is non-contributory, and she has no known allergies. The purpose of this report is to present the relevant patient findings noted in this case including the clinical and radiographic exam, differential diagnosis, and referral for definitive treatment. A literature review of intra-oral soft tissue lesions in pediatric patients will also be presented.
-

February in Santiago Atitlan, Guatemala
Grace Milburn
Describes her experience working in Santiago Atitlan, Guatemala.
-

Space Loss After Removal of a Band and Loop Space Maintainer: A Case Report and Review of the Literature.
Kaitlin Carlson, Robin Onikul, Amy Burleson, Jenna Sparks, Neena Patel, and Brenda S. Bohaty
Premature loss of a first primary molar can occur due to a multitude of reasons, including caries and infection. When this occurs and restoration of the affected primary tooth is not possible, the AAPD recognizes space maintenance as a “Best Practice” to prevent loss of arch length, width, and perimeter after extraction. However, reports suggest that with proper intercuspation of first permanent molars, space loss from premature loss of a first primary molar is minimal and space maintainers in that area may not be needed. This case report details an 8-year-old female who had significant space loss between the mandibular primary canine and mandibular second primary molar after removal of her band-and-loop space maintainer post-eruption of tooth #19. Patient’s medical history is non-contributory, and she has no known allergies. This report reviews the pertinent literature regarding space management in the mixed dentition and outlines factors to be considered in making clinical decisions regarding such management.
-

The Impact of Health-Related Social Needs on Health Outcomes among Youth Presenting to a Midwest Pediatric Diabetes Clinic Network
Jasmine Roghair, Emily DeWit, Katelyn Evans, Mitchell Barnes, Heather Feingold, Samantha Jacob, Courtney M. Winterer, Jeffrey D. Colvin, Mark A. Clements, Shilpi Relan, and Kelsee Halpin
Objective: Screening for health-related social needs (HRSNs) is recommended as part of routine diabetes care given the strong impact of social factors on health outcomes. Our objective was to compare diabetes-related health outcomes among youth presenting to a tertiary diabetes center based on whether they screened positive or negative for HRSNs at a routine clinic visit. Methods: Baseline data were collected from patients whose parent/guardian completed a HRSN screen as part of their child’s diabetes clinic intake from 9/1/21 to 8/30/22. The screen is a 6-item questionnaire adapted from the Accountable Health Communities HRSNs Screening Tool. Longitudinal data were analyzed from the time of first screen through 8/30/23. Comparisons were made using chi-square or t-test. Results: Among 1880 unique respondents, 14% were positive for at least one HRSN. The most common HRSN was food insecurity (72%). A positive HRSN screen was more likely in non-white minorities (22% vs. 11% non-Hispanic white youth), publicly insured (22% vs. 8% privately insured), youth with a type 2 diabetes diagnosis (32% vs. 12% with type 1 diabetes), all p<0.001. Those with a positive vs. negative HRSN screen at baseline were more likely to have any A1c > 10% (32% vs. 19%), any A1c >13% (9% vs. 4%), at least one no-showed appointment (41% vs. 26%), a positive PHQ4 screen for anxiety/depression (22% vs. 11%), and a second positive HRSN screen (29% vs. 5%), all p<0.001, during the follow up period (mean 14.8 =/- 2.0 months). They were more likely to have an ED visit (17% vs. 12%, p 0.025), though DKA admissions were not significantly different between the groups (6% vs. 4%, p=0.15). Insulin pumps (58% vs. 75%) and continuous glucose monitors (CGMs) (58% vs. 76%) were also less utilized throughout the study period in those screening positive for a HRSN at baseline, p<0.001. Conclusion: Youth with positive HRSN screenings during diabetes clinic appointments experience suboptimal diabetes-related outcomes, including higher A1c levels, increased rates of missed appointments, anxiety/depression, ED visits, and less utilization of diabetes technologies. This highlights the importance of addressing social risk factors when treating youth with diabetes to enhance equity in delivery of care and improve health outcomes.
-
The Role of Adverse Childhood Events on the Progression of Chronic Kidney Disease in Children: A CKiD Study
Ana Cortez, Matthew Matheson, John Cowden, Bradley Warady, and Darcy K. Weidemann
There is a paucity of research on the relationship between adverse childhood events (ACEs) and chronic kidney disease. The effect of ACEs on the long-term health outcomes of cardiovascular disease, cancer, and chronic lung disease first emerged in a paper published in 1998. The National Institutes of Health sponsored the ACE Study, which Kaiser Permanente carried out in California. The study used a 17-question survey addressing seven exposures: psychological, physical, contact-sexual abuse, substance abuse, mental illness, mother being treated violently, and criminal behavior in the household. The results revealed a strong relationship between childhood exposure to ACEs and health outcomes. When individuals experienced four or more such exposures, the odds ratio ranged from 1.6 to 3.9 for ischemic heart disease, cancer, stroke, chronic bronchitis or emphysema, and diabetes (Vincent et al., 1998). This monumental analysis remains a focal point in research more than twenty years after the initial publication of its results. Since then, numerous studies have investigated how childhood exposures can increase disease risk. Surprisingly, chronic kidney disease (CKD) has received little attention in terms of the influence of ACEs in the pediatric and adult populations. Objective Specific Aim #1: Characterize the prevalence of ACEs in the CKiD cohort. Specific Aim #2: Characterize disease progression among those who experienced ACEs compared to those who have not.
-
Thyroid Dysfunction in Patients Receiving Immune Checkpoint Inhibitors
Emily Metzinger, Jennifer Boyd, Julia Broussard, and Christopher Klockau
Objectives: The use of immune checkpoint inhibitors (ICIs) in cancer treatment is increasing. Literature about endocrinopathies associated with ICIs in children is limited. This study investigates ICIs and thyroid dysfunction in pediatric patients at one institution.
Methods: Retrospective chart review of patients ages 1 to 19 was completed who received any of the following ICIs between January 2000 and November 2023: PD-1 inhibitors (nivolumab or pembrolizumab), PD-L1 inhibitors (durvalumab or atezolizumab), and CTLA-4 inhibitors (ipilimumab or tremelimumab). Patients were excluded if thyroid function tests (TFTs) were not available to review or if patients passed away within 30 days of ICI initiation. TFTs were considered abnormal if they were outside the reference range for age.
Results: Data analysis included nineteen patients. Of these, thirteen patients received nivolumab and three patients received multiple ICIs. Average age at time of ICI initiation was 14.9 years. Baseline TFTs were obtained in fourteen patients at ICI initiation and ten of these patients also had TFTs checked after initiation. Abnormal TFTs were seen in five patients after starting ICI therapy; four of these patients received nivolumab and one received pembrolizumab. Average time to thyroid dysfunction from ICI initiation was 3.3 months. Levothyroxine (LT4) was started in three patients for persistent abnormal TFTs (one patient had central hypothyroidism and two patients had primary hypothyroidism). Average time to LT4 treatment was 4.2 months. Two patients developed hypothyroidism prior to starting ICI therapy. Of these, one patient developed hyperthyroidism 2.9 weeks after ICI initiation. Hyperthyroidism resolved with temporary LT4 discontinuation, followed by restarting LT4. Six patients had baseline abnormal TFTs with ICI initiation of which two patients required levothyroxine.
Conclusions: Thyroid dysfunction can be seen within several months of ICI initiation, particularly PD-1 inhibitors. Hypothyroidism and hyperthyroidism were seen, though hypothyroidism was more common. This study supports monitoring TFTs (both TSH and free T4 levels) at baseline and during therapy with ICI. Limitations to our study include small patient population. Future studies should look at development of other endocrinopathies in children such as diabetes mellitus or adrenal insufficiency.
-
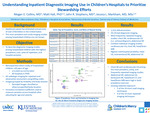
Understanding Inpatient Diagnostic Imaging Use in Children’s Hospitals to Prioritize Stewardship Efforts
Megan Collins, Matt Hall, John R. Stephens, and Jessica Markham
Background: Healthcare waste, including overuse of treatments or testing such as unnecessary diagnostic imaging, has estimated annual costs of over $760 billion in the United States. The most prevalent and costly imaging studies among hospitalized children are not known. Objective: To describe diagnostic imaging studies among hospitalized children with the highest prevalence, cost, rates of repetition, and hospital variation to help inform de-implementation efforts. Design/Methods: We performed a retrospective cohort study of children <18 years of age hospitalized from 1>/1/2021 to 12/31/2022 across 45 hospitals in the Pediatric Health Information System. We identified all radiologic imaging for inpatient and observation encounters using billing codes. We grouped images by modality and body location, and excluded images classified as other/unspecified body location. The intraclass correlation coefficient was used to measure variation across hospitals in imaging use after adjusting for age and severity. Higher numbers indicate a higher degree of variation. Results: We identified 1,523,343 encounters; 59.1% had diagnostic imaging (Table 1). The most prevalent diagnostic imaging studies were chest x-ray (XR), abdominal XR, and echocardiogram. The images most frequently repeated were chest XR, echocardiogram, and abdominal XR. The costliest individual diagnostic imaging studies were echocardiogram, chest XR, and head/brain MRI (Table 2). Although chest XR was among the least expensive imaging modalities per unit cost, given the high prevalence of use and repeat use it was one of the costliest tests overall. Head US, interventional XR, and abdominal US had the highest variability of use between hospitals (Table 2, Figure). Conclusion(s): Chest XR and echocardiograms were among the most prevalent, costly, and frequently repeated imaging studies. Abdominal XR, abdominal ultrasound, bone/joint XR, head/brain CT, and head/brain MRI were high in both prevalence and cost among hospitalized children. Five of the 10 most commonly used imaging techniques and four of the 10 most commonly repeated imaging techniques expose children to ionizing radiation. These results could help identify areas that should be targeted to reduce radiation exposure, improve care, and decrease costs for hospitalized children.
-

Anesthetic and Multidisciplinary Management of a 2-staged Liver Transplant
Kasey Brooks, Lisa Conley, and Brandon Layton
We present a case of a 2 staged liver transplant on a 12-month-old 8kg male with newly diagnosed mitochondrial depletion syndrome causing acute liver failure, refractory lactic acidosis, and cardiopulmonary collapse requiring ECMO. The patient’s past medical history at the time of presentation included history of prematurity at 32 weeks, developmental delay, and a brother with an undiagnosed pancreatic disorder. The patient was brought in by parents to the emergency department with a cough, minimal PO intake for 5 days, and increased fatigue who was found to be URI positive. Initial labs were concerning for anemia, elevated bilirubin, elevated AST/ALT, hyponatremia, coagulopathy, and metabolic acidosis secondary to an elevated lactate of 11.5 mmol/L. An ultrasound of the liver showed hepatocellular inflammation with small perihepatic and pericholecystic fluid. He was admitted to the floor for observation and continued testing. 4 days after admission he had an acute decompensation due to fulminant liver failure and persistent severe lactic acidosis requiring intubation, resuscitation, and VA ECMO support. The leading diagnosis was that he had an inborn error of metabolism causing liver necrosis. Whole exome sequencing was performed to better delineate the cause of his persistent lactic acidosis and liver failure. Due to the dire nature of the patient's medical course, a multidisciplinary meeting was held and he was listed status 1A for a liver transplant due to a necrotic liver. The operative plan was for the transplant surgery team to perform a hepatectomy with return to the ICU post operatively to allow improvement in his physiology and for his lactic acidosis to correct itself and then receive a whole liver transplant the following day. The patient remained intubated and sedated and was taken to the operating room with the OR nursing staff, PICU team, ECMO staff, CRRT nurse, anesthesia team, and surgical team. He was then terminally extubated 2 months after his initial presentation.
-
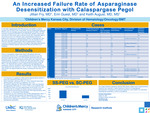
An Increased Failure Rate of Asparaginase Desensitization with Calaspargase Pegol
Jillian Fry, Erin M. Guest, and Keith J. August
Background: In late 2022, pegaspargase (SS-PEG) became unavailable to patients younger than 22 years in the United States, leaving calaspargase pegol (SC-PEG) as the only available long-acting asparaginase formulation. SC-PEG has been compared to SS-PEG in two randomized, pediatric clinical trials and found to have similar rates of adverse events with comparable rates of event-free survival. Our institution uses a desensitization protocol for patients who experience a hypersensitivity reaction to asparaginase. Here we review our experience with desensitization since the transition to SC-PEG from SS-PEG. Objectives: To compare the rate of hypersensitivity reactions, success of desensitization protocols, and need for alternative asparaginase preparations between patients receiving SC-PEG and SS-PEG at our institution. Design/Method: This is a retrospective, single center study of pediatric patients who received at least 2 doses of SC-PEG between November 2022 and December 2023. Results: We report on 26 patients with acute lymphoblastic leukemia and lymphoblastic lymphoma who received at least two doses of SC-PEG. The frequency of a grade 2 or higher clinical hypersensitivity reaction in those who received SC-PEG was 42.3% (n=11). Silent inactivation, defined as serum asparaginase activity (SAA) <0.1 IU/mL measured seven days following dosing, occurred in an additional 7.8% (n=2). Ten patients underwent SC-PEG desensitization using a protocol that was identical to our previously published protocol using SS-PEG (August, et al., Ped Blood Cancer, 2020). In the desensitization protocol, patients were premedicated with prednisone, cetirizine, famotidine, and montelukast. SC-PEG 2500 IU/m2 was divided into three fractions of 1:100, 1:10, and 1:1 dilution. Each fraction was infused over approximately 60 minutes, increasing the rate every 15 minutes. Desensitization was tolerated with appropriate SAA levels (0.1 IU/mL) in 30% (n=3) of patients, 60% tolerated the infusion but had inappropriately low AA levels (n=6), and one patient did not complete the infusion due to an adverse event. Six patients received Rylaze following SC-PEG hypersensitivity, silent inactivation, or unsuccessful desensitization. Compared to our prior experience with SS-PEG desensitization where 17 out of 21 attempts were successful with appropriate SAA levels (August, et al., ASH, 2022), our success rate using SC-PEG (7 failures out of 10 attempts) is significantly less (p=0.013), leading to an increase in the use of an alternative asparaginase preparation. Conclusion: Our single institution experience with SC-PEG shows a high rate of hypersensitivity reactions, a high likelihood of failure of asparaginase desensitization compared to our historical experience, and the frequent need to switch to an alternative asparaginase preparation.
-

Congenital Heart Defects and Autism: Understanding the Breakdown of Associated Risk Factors In A Clinically Referred Sample
Elizabeth Raines, Amanda Strasser, Amanda Manderfeld, Paul Glasier, and Elizabeth J. Willen
Background: Children with Congenital Heart Disease (CHD) have higher odds of developing social difficulties and/or an Autism Spectrum Disorder (AuSD) than the general population (i.e., ~10% vs. ~1%). However, there is a paucity of nuanced understanding of specific drivers of the increased rates of AuSD in extant literature. The purpose of this study is to identify the rates of co-occurring cardiac, neurological, and genetic conditions to better understand associated risk factors in a patient sample from a medium-size children’s hospital. Methods: Our population includes a clinically referred sample of children (i.e., medical history of CHD and neurodevelopmental risk) under 18 who received a diagnosis of AuSD through neuropsychological evaluation at Children’s Mercy Kansas City (CMKC) between 01/2021 and 12/2022 (N = 356 total sample; N = 50 AuSD). Results: Analyses explored rates of co-occurring cardiac, neurological, and genetic conditions among children with AuSD (10.39% of the overall CHD sample). In this sample of children with CHD and AuSD, the following prevalence rates represent the largest categories of cardiac, neurological, and genetic comorbidities, respectively: 1) Ventral Septal Defect (VSD) (24%), 2) abnormal imaging/ECMO (12%), and 3) genetic variant of unknown significance and 22q11.2 deletion (both 4%). Additional rates of AuSD and specific co-occurring conditions will be presented in detail. Conclusion: Increased recognition of the higher risk of AuSD in the CHD population is emerging. Understanding the rates of different types of co-occurring cardiac, neurological, and genetic conditions will further improve patient centered care. It is imperative that providers include regular AuSD screening in clinics to ensure appropriate access to evaluation, treatment, and family support.
-

Diagnosis of Mosaic RASopathy in a Child with Rhabdomyosarcoma
Meagan Vacek, Paige Johnson, Midhat S. Farooqi, Kristi M. Canty, Dihong Zhou, Brendan Lanpher, Wendy Allen-Rhoades, and Erin M. Guest
Background: Phacomatosis pigmentokeratotica (PPK) is a subtype of epidermal nevus syndrome characterized by the co-existence of a sebaceous nevus and a speckled lentiginous nevus and described in approximately 30 cases in literature. PPK is now recognized as a mosaic RASopathy due a postzygotic mutation in the Ras-Raf-MEK-ERK pathway. RAS variants are also known to contribute to tumorigenesis, in some pediatric cancers, including rhabdomyosarcoma. Objective: Describe the presentation and evaluation of a child with pelvic rhabdomyosarcoma and evolving skin lesions found to have a rare mosaic-RASopathy. Design/Method: Case Report Results: The patient is a former 32-week premature female who presented to dermatology clinic at 2 months of age for birthmarks on her back and right shoulder. She was diagnosed with epidermal nevi and congenital melanocytic nevi with the possibility of having an epidermal nevus syndrome. At 4 months of age, she was hospitalized for obstructive renal failure secondary to a pelvic mass. Biopsy of the mass was diagnostic for embryonal rhabdomyosarcoma with gain of chromosomes 2, 3, 5, 8 and 11, and copy-neutral loss of heterozygosity of 11p15.5. Molecular testing revealed HRAS G13R mutation in the tumor, but not in a blood sample. Five months after her cancer diagnosis she underwent tumor resection and skin biopsy. Whole exome sequencing of the skin biopsy showed a variant of uncertain significance in PORCN gene. While receiving chemotherapy and post-treatment, her skin lesions continued to evolve with increased size and number of nevi. A single nucleotide polymorphism-based microarray was performed on blood to assess for any germline copy number variants but was negative. Due to ongoing concerns for PPK, she underwent her second and third skin biopsies. The two lesions biopsied and showed the same HRAS G13R mutation as her tumor, confirming a diagnosis of a mosaic RASopathy almost 2 years after her first dermatology visit. Conclusion: Mosaic RASopathies remain a diagnostic challenge. Tissue involvement can be varied and subtle, DNA sequencing of the blood is often negative, and phenotypes can depart from germline RASopathies, even when caused by the same mutation. With only case reports and small case series describing an association between cutaneous mosaic RASopathies and rhabdomyosarcoma, there is a need for further awareness of this association as it may impact treatment decisions. Also, despite cancer screening guidelines for germline RASopathies being well established, they are not available for mosaic cases, leading providers to question future malignancy risks in this patient population.
-

Early Cholestasis and Vitamin K Deficiency Secondary to Biliary Atresia presenting as Coagulopathy and Thymic Hemorrhage
Abbey Elsbernd and Lauren Amos MD
Background Bleeding and progressive coagulopathy are established symptoms of early cholestasis, including extrahepatic biliary atresia. We present a patient with bleeding secondary to vitamin K deficiency and cholestasis-induced fat malabsorption with unusual presentation of mediastinal mass. Objective Describe a case of late-onset vitamin K deficiency and cholestasis ¬¬presenting as jaundice and coagulopathy with associated bleeding into thymic structures Design/Method Case report Results A 4-week-old term male infant was brought to the ED with fussiness and bruising. Prior to presentation, he was afebrile and followed regularly with his primary care provider for jaundice below phototherapy thresholds. Infant received vitamin K at birth. In the ED, infant was tachypneic with retractions and grunting. Physical examination was notable for diffuse jaundice and two 1 cm bruises along shoulder and midline thoracic spine. No hepatosplenomegaly was noted. Chest x-ray was significant for mildly widened mediastinum. Labs demonstrated elevated WBC 19.68 x10(3)/mcL, Hgb 10.8 gm/dL, Platelet count 287 x10(3)/mcL. LFT notable for mixed direct/indirect hyperbilirubinemia with total bilirubin 11.1 mg/dL, direct bilirubin 5.6 mg/dL, indirect bilirubin 5.5 mg/dL. DAT was negative. Coagulation studies were significantly abnormal, with PT >125 sec and aPTT >250 sec; INR was unable to be completed. Fibrinogen was 406 mg/dL. A repeat set of coagulation studies were similarly abnormal. Infant received 2 mg vitamin K for three days, 50 IU/kg KCentra, and 15 mg/kg fresh frozen plasma. Factors VII and IX were low, factor VIII was high, and factor V was normal consistent with late-onset vitamin K deficiency bleeding. Coagulation studies normalized after these interventions. An echocardiogram and computed tomography scan of the chest were obtained due to respiratory distress identifying an anterior mediastinal mass bifurcating the thymus. Due to concern for solid appearance of the mass, a biopsy was completed demonstrating only normal thymic tissue, suggestive of bleeding into his thymic structures as cause of mass. He was able to be discharged with ongoing stability in coagulation labs but with ongoing fat malabsorption and persistent cholestasis. He followed closely with hepatology outpatient and was ultimately diagnosed with biliary atresia with Kasai procedure completed at 8 weeks of age. Conclusion Bleeding associated with Vitamin K deficiency and cholestasis may present variably in neonates, including intracranial bleeding, bruising, and coagulopathy; in this case, our patient presented with thymic bleeding and mediastinal mass. Vitamin K deficiency is correctable in the acute setting, however, early identification and further evaluation is indicated to address underlying causes of cholestasis.
-

Hearing Loss In Children With 22q11.2 Deletion Syndrome
Lori Yaktine, Amanda Moore, Jamie Hamm, Blaine Crowley, Meghan Tracy, Janelle R. Noel-Macdonnell PhD, Kim Graiser, Bernice Marrow, Hansoo Song, Srivats Narayanan, Nikita Raje, Donna McDonald-McGinn, and Jill M. Arganbright
22q11.2 deletion syndrome (22q11.2DS) is the most common microdeletion syndrome, with most recent published prevalence of 1:2,140 live births. Hearing loss is common in children with 22q11.2DS and has been reported to occur in 32-60% of people. Hearing loss is typically conductive in nature secondary to chronic eustachian tube dysfunction and chronic otitis media with effusion (COME). Close monitoring of hearing and the middle ears is recommended to detect COME and the need for ear tubes. Additionally, there is a high prevalence of speech delay in children with 22q11.2DS, stressing the importance of close audiometric evaluation and medical intervention as appropriate. While prior studies confirm a relationship between hearing loss and 22q11.2DS in children, there is a lack of data regarding frequency, type, and specific features of hearing loss for children with this syndrome.
-

Increasing Palliative Care Team Involvement in Pediatric Hematopoietic Stem Cell Transplant Patients
Meagan Vacek, Lisa Tarbell, Melissa List, Erin Hall, Jennifer Linebarger, Kelstan Ellis, Gina Jones, and Joel Thompson
Background: Palliative care facilitates communication, helps with physical and psychological symptom management, and assists in goals of care and advance care planning discussions.1 Multiple organizations, including the American Academy of Pediatrics and American Society of Clinical Oncology encourage palliative care engagement and their involvement with hematopoietic stem cell transplant (HSCT) patients has been shown to be beneficial as HSCT is associated with a high degree of morbidity and possible mortality.2-3 Objective: To increase the number of PaCT consults for patients receiving HSCT for our targeted diagnoses from 48% to 75% by December 2023. Methods: Chart review was conducted for patients who underwent HSCT from July 2020 to July 2022. Demographics documented included reason for and date of HSCT, date of PaCT consult and living status. A targeted diagnosis list was compiled based on which patients were felt to benefit most from palliative care involvement: relapsed or refractory leukemias and lymphomas, myelodysplastic syndrome, high risk myeloid leukemias and metabolic disorders, such as Hurler syndrome. The first plan-do-study-act (PDSA) cycle included discussion of the project at division meetings and education regarding palliative care and evidence of its involvement in HSCT patients. The second PDSA cycle involved revision of the HSCT referral form to include the question “Is PaCT consulted.” During this time, PaCT also started attending the weekly transplant team meetings to discuss current and upcoming patients. Results: Baseline data from July 2020 to July 2022 revealed 48 patients underwent HSCT, 25 of whom had a targeted diagnosis. PaCT met 12 of the 25 patients (48%). From the initiation of the project on 1/1/23 to 11/30/23, 14 patients with a targeted diagnosis underwent HSCT. Eight of the 14 patients (57%) received a PaCT consult. Conclusions: Palliative care involvement in pediatric oncology is well established, but its role in HSCT patients continues to be explored. As HSCT patients receive more intense therapy, have frequent deaths in intensive care units and can have limited opportunity for end of life planning due to rapidly changing clinical courses, early integration of PaCT could allow for decreased symptom burden and distress for both patients and families.4 Future PDSA cycles to further increase involvement include adding PaCT consultation to the transplant evaluation order set in the electronic medical record and review of the comments on the completed HSCT referral forms to identify possible barriers in the PaCT consultation process.
-
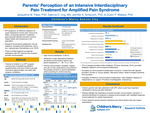
Parents’ Perception of an Intensive Interdisciplinary Pain Treatment for Amplified Pain Syndrome
Jacqueline Pabis PhD, Sabrina Ung, Jenny Scheurich, and Dustin Wallace PhD
Introduction: Intensive interdisciplinary pain treatment (IIPT) is an effective treatment for youth impaired by chronic pain (Claus et al., 2022). IIPT programs incorporate parents in treatment, as parental distress has been found to impact health and functioning in youth with chronic pain. Research has suggested parent satisfaction may be related to increased child adherence, and in turn, reduced pain (Gorodzinsky et al., 2012). There is limited research on parental satisfaction with IIPT and the role of parent-provider communication. Method: Parents (n=99) of children in an IIPT program completed questionnaires related to treatment satisfaction, parent-provider communication (e.g., provider listened carefully, provider showed respect, provider used clear explanations), and perceived child functioning/mental health. Questionnaires were completed anonymously, approximately one week after program completion. Descriptive and inferential statistics were conducted, with qualitative analysis of parents’ written feedback providing additional context. Results: Descriptive analyses revealed overall strong ratings for communication across providers and satisfaction with the program. Correlations showed greater ratings of communication were associated with greater program satisfaction, as well as with higher perceived child functioning and mental health. Forward linear regression, controlling for perceived child functioning, revealed that among communication variables, respect from the provider (b=.39, p=.01) and use of clear explanations (b=.32, p=.01) accounted for the greatest variance in parent satisfaction (R2=58%). Qualitative analyses found most parents considered IIPT a “life changing,” positive experience. Additional feedback focused on logistics (e.g., insurance/billing), child experience (e.g., intensity level), parent involvement (e.g., increased parent therapy), and post-program transitions (e.g., to school). Conclusions: Parents overall have high satisfaction with IIPT, which could have important ramifications for family participation during and after treatment. Results highlight the importance of parents feeling respected by providers and the family’s perception that the provider used clear explanations. Parents’ qualitative feedback will be discussed in detail to consider further potential enhancements.
-
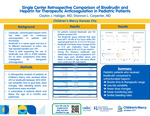
Single Center Retrospective Comparison of Bivalirudin and Heparin for Therapeutic Anticoagulation in Pediatric Patients
Clayton Habiger and Shannon L. Carpenter
Background: The pharmacological choice for continuous anticoagulation therapy in pediatric patients has classically been unfractionated heparin. However, with heparin there are risks of treatment resistance in pediatrics given differences in developmental hemostasis, and contemporary medications such as bivalirudin offer a valuable alternative. Bivalirudin binds to thrombin and has shown encouraging results compared to heparin in pediatric patients receiving ECMO, but no comparison has been made in patients receiving therapeutic anticoagulation. Three years ago, Children’s Mercy Pediatric Hematology department encouraged bivalirudin use over heparin use for therapeutic anticoagulation requiring a continuous infusion. Objectives: Compare clinical and laboratory outcomes in patients receiving bivalirudin and continuous heparin for therapeutic anticoagulation secondary to a thrombotic event. Methods: A retrospective chart review between 1/1/13 to 12/31/22 was performed and looked specifically at patients who had a pediatric hematology consult for therapeutic anticoagulation who were not on ECMO or CRRT. Patients who were on prophylactic dosing or were using the medication for prophylaxis at therapeutic ranges were excluded. Results: 46 patients received bivalirudin during this time while 135 patients received heparin. The time to therapeutic range was significantly shorter in the bivalirudin group compared to the heparin group (3.7 hours vs 18.6, respectively). Additionally, the bivalirudin group had fewer monitoring labs (0.09 vs 0.15), RBC transfusions (0.0019 vs 0.0097), plasma transfusions (0.00074 vs 0.0048), and dose changes (0.025, 0.54) per medication hour (all p<0.05). Both groups had similar rates of bleeding events (6.5% vs 16.3%; p=0.52) despite bivalirudin having more patients who had concurrent bleeding at the time of anticoagulation induction (21.7% vs 5.2%; p<0.05). None of the bivalirudin patients failed to achieve a therapeutic level while 18.6% of heparin patients required a change in anticoagulation due to failure to achieve therapeutic goal. Finally, when monitoring labs (heparinased PTT and Anti-Xa) were standardized to a percentage of goal there was significantly less variation in the bivalirudin group (p<0.001). The average age was older in the bivalirudin group (9.9 vs 1.1) so to account for this, patients were subdivided into under and over 6 months of age. There were 13 bivalirudin and 64 heparin patients who were under the age of 6 months and 33 bivalirudin and 71 heparin subjects older than 6 months of age. The same differences were noted in both subgroups (shorter time to therapeutic range, fewer monitoring labs, RBC transfusions, and dose changes, and more lab monitoring variability). There was no difference in bleeding events in both subgroups when compared with their age cohort. The bivalirudin group had fewer patients with congenital heart conditions (11% vs 47%) and this difference was still noted after subdividing the age groups. Conclusions: Pediatric patients who received bivalirudin had shorter time to a therapeutic range, less lab variability, fewer dose changes, fewer monitoring labs and fewer transfusions with similar bleeding rates compared to patients who received unfractionated heparin.
-

Something's Gnawing at Me
Catharine Kral and Brian Harvey
17-year-old female presented to Sports Medicine clinic with a chief complaint of bilateral hip pain and difficulty walking who was found to have bilateral ovarian teratoma.
-

Speeding Up Time: An Old Back in a Young Athlete
Carey Wagoner and Greg Canty
Case of a 16 year old female competitive dancer with chronic back pain. Previous diagnosis of mechanical low back pain being treated by PT without improvement. Further workup demonstrated bilateral spinal synovial cysts at L4/L5 facet joints. Patient underwent IR guided aspiration and steroid injection with resolution of her symptoms and ultimately returned to dance.
-
Telehealth Implementation of a Young Adult IBD Clinic: Uptake, Benefits to Patient Care, and Challenges
Angela Combs MA, Alaina Linafelter, Jordan Sevart, and Michele H. Maddux
Introduction: Since the COVID-19 pandemic, pediatric psychologists have been at the forefront of telemedicine expansion to ensure access for patients and families to needed mental health services. This has required adaptations across the care continuum – from scheduling to service delivery to documentation. This poster aims to summarize the telehealth (TH) application of a Young Adult IBD Clinic (YAC-IBD) that provides transition preparation to youth with Inflammatory Bowel Disease (IBD). Methods: In April 2020, the YAC-IBD was converted from in-person visits to a virtual visit format. Since then, 119 youth ages 17-21 (inclusive) have been seen in this clinic. This clinic is staffed by a pediatric psychologist, nurse practitioner, and pharmacist, all of whom are programmatically dedicated to youth with IBD. As part of YAC-IBD, youth and caregivers complete a standard battery of psychosocial screeners (not described herein). Qualitative feedback from patients/caregivers and clinic providers was obtained on feasibility, challenges, and solutions to converting multidisciplinary visits to a telemedicine format. Opt-in to be seen in the YAC-IBD, no-show, cancelation, and rescheduling rates were also evaluated. Results: Qualitative feedback from patients/caregivers revealed preference for TH visits, due to fewer scheduling constraints and the convenience of seeing their provider from their college campus. Feedback from clinic providers revealed the benefit of less repetition across providers, improved access, and more collaborative treatment planning. Challenges include distractions, connectivity issues, and privacy concerns. Opt-in rate increased by approximately 20.0%. No-show rates from 2-years prior to 2-year following TH implementation decreased from 25.7% to 21.0%. Cancelation rates decreased from 37.61% to 23.13%, and rescheduling rates decreased from 39.45% to 30.63%. Conclusions: While the transition from in-person to TH in the YAC-IBD involved logistical challenges, data on satisfaction and show rates suggest that TH implementation is a promising format for transition planning and support to youth with IBD.