These posters have been presented at meetings in Children's Mercy and around the world. They represent research that was done at the time they were created, and may not represent medical knowledge or practice as it exists at the time viewers access these posters.
-
A Case of Early Pediatric-Onset Multiple Sclerosis
Mellanie De Guzman and Marcy Vandament
Pediatric-onset multiple sclerosis (POMS) is a central nervous system neurodegenerative disease impacting individuals who experience symptom onset prior to the age of 18-years-old.17 Children and adolescents diagnosed with POMS prior to 16-years-old are considered as early POMS cases. 1,6,10,11, 18 The current case study presents an 11-year-old boy, “Patient A,” who was diagnosed with POMS at 10-years-old. Common neurocognitive weaknesses and behavioral concerns seen in this patient population include deficits in language (receptive, expressive, verbal fluency), memory, attention, executive functions, processing speed, visual-motor/fine-motor coordination/dexterity, depression, anxiety, and fatigue.2-5,15,20 Results from testing demonstrated mild weaknesses in abstract reasoning and fine motor coordination/dexterity. Qualitative concerns surrounding executive functioning and mild depression were reported. Overall, no significant cognitive or behavioral concerns were revealed. Therefore, no additional diagnoses were provided aside from Patient A’s historical diagnosis of POMS. Establishing a neurocognitive baseline for patients diagnosed with early POMS is pivotal for the monitoring of their cognitive, behavioral, and adaptive functioning over time. Incorporation of a pediatric neuropsychologist as part of the patient’s treatment team and the implementation of comprehensive neuropsychological evaluations can support this goal of longitudinal comparison.
-

Scoring Large Muscle Movements in Pediatric Sleep Studies: An Educational Module for Sleep Technologists
Shauna Michelle VanDoren and David G. Ingram
Introduction Restless Sleep Disorder (RSD) has recently been recognized as a distinct sleep disorder, with Large Muscle Movement (LMM) scoring being a crucial component of its diagnostic criteria. This project aimed to develop and implement an online educational module to enhance the knowledge and skills of sleep technologists to accurately score LMMs. Methods We constructed an online learning module that included training on the identification and scoring of LMMs in pediatric sleep studies. The module consisted of a 10-question pre-assessment, the educational content (which explained the background of RSD diagnosis, the role of LMMs in diagnostic criteria, and current scoring rules), a repeat of the 10 questions for post-assessment, and a feedback section regarding the module and LMM scoring in general. Results Preliminary results indicate a significant improvement in the accuracy and consistency of LMM scoring among sleep technologists who completed the module. The average post-module assessment scores showed a marked increase compared to pre-module scores, with total scores on the 10-question learning assessment increasing from 63.3+/-20.6% pre-module to 90.0+/- 8.9% post-module (p=0.017). Eighty percent of technologists agreed or strongly agreed with the statement that “As a result of taking this course I am confident I can recognize the clinical characteristics, symptoms, and diagnostic criteria of RSD.” Similarly, 60% agreed or strongly agreed with the state that “As a result of taking this course, I am confident I can accurately apply scoring guidelines for LMM events in sleep studies.” Feedback from technologists regarding the module itself, as well as questions and suggestions regarding LMM scoring in general, provided valuable information for potential future revisions of scoring rules. Conclusion An online educational module significantly improved the knowledge and ability of sleep technologists to score LMMs accurately, thereby aiding in the diagnosis of RSD. This initiative highlights the importance of continuous education and training in maintaining high standards of care in pediatric sleep studies.
-

When Macroglossia is not Beckwith-Wiedemann: A Case of an Infant with Congenital Central Hypoventilation Syndrome
Shauna Michelle VanDoren and Samira Naime
Introduction Congenital central hypoventilation syndrome (CCHS) is a rare genetic disorder caused by the mutation of the paired-like homeobox 2B (PHOX2B) gene that leads to alveolar hypoventilation during sleep and at times while awake. The majority of patients with CCHS have polyalanine repeat mutations (PARM) whereas 10% have non-PARM (NPARM). Of those with NPARM, less than 1% are caused by whole gene deletion. NPARM is associated with more severe phenotypes; however, some may have variable penetrance causing variable presentation within families. Report of case(s) Our patient is a 4-month-old infant born at 32 weeks in an outside hospital and transferred to our tertiary NICU at 10 weeks of age due to feeding difficulties, respiratory distress, hypoxemia, macroglossia and concern for Beckwith-Wiedemann syndrome. Upon transfer, she was on 2L of oxygen (FiO2: 0.3) via high flow nasal cannula. During her stay, she was noted to have hypoventilation which was thought to be secondary to upper airway obstruction. Upper airway evaluation by ENT revealed mild laryngomalacia for which supraglottoplasty was performed. Drug induced sleep endoscopy (DISE) revealed macroglossia with posterior displacement of the epiglottis causing obstruction. Due to concerns for obstruction and persistent hypoxemia, she was referred for a polysomnogram (PSG). The study was started on room air, but 1/4L of oxygen via low flow nasal cannula (LFNC) was initiated after 6 minutes due to persistent hypoxemia and hypoventilation. PSG showed an apnea hypopnea index (AHI) of 18/hour, central apnea index (CAI) of 11/hour with persistent nocturnal hypoventilation based on ETCO2, transcutaneous CO2 monitor (TCM) and blood gas (ETCO2 > 50mmHg for 85% of total sleep time (TST), max ETCO2: 62mmHg, TCM>50mmHg for 96% TST, peak TCM: 70mmHg). Given these findings, recommendations were made to obtain PHOX2B gene testing and obtain neurologic workup. Exome sequencing showed deletion of the PHOX2B gene consistent with CCHS. Conclusion A high suspicion for CCHS should be present in patients with central apnea and hypoventilation. Many children with CCHS may be missed due to complex genetic testing and variation in clinical presentation.
-

A single center qualitative study to improve coordination of follow-up care for patients diagnosed with Abusive Head Trauma
Ruairi Smith-Dewey, Elise Wright, Daniella Donofrio, Hannah Goebel, and Sara Kilbride
Introduction: Children diagnosed with abusive head trauma (AHT) have subsequent long-term developmental, behavioral, and medical consequences resulting in increased medical system utilization. There were 16 overall potential needs identified, with a single patient having 12. In 2023 at Children’s Mercy Hospital (CMH), 47% (8/17) of patients with AHT had < 50% of follow-up needs addressed at time of discharge. None had 100% of follow-up needs addressed. Needs not being addressed included need not identified or written documentation for need of follow-up without subsequent referral placed/appointment scheduled. Project goal was all follow-up needs to be addressed for at least 50% of children with AHT by January 2025. Methods (include PDSA cycles): Children admitted to CMH from January 2024-December 2024 and diagnosed with AHT by the Safety, Care & Nurturing (SCAN) team were included. Interventions were designed and implemented by a multidisciplinary team to address barriers including variation in scheduling process per specialty, lack of knowledge, and changing caregivers. • PDSA 1 (1/1/24): SCAN added standardized list of potential follow-up needs to documentation. • PDSA 2 (2/1/24): Trauma NP placed ophthalmology outpatient referrals. • PDSA 3 (3/1/24) Social work placed and documented early intervention referrals. Transitioned to SCAN RN responsibility. • PDSA 4 (4/10/24): AHT caregiver handouts with description of all potential follow-up needs added to discharge instructions. • PDSA 5 (12/11/24): AHT Evidence Based Practice guideline created including follow-up needs. Appointments and referrals were tracked by the author. QI tools used included fault tree, fishbone, and PICK Chart. Results: In 2024, 27 children were diagnosed with AHT by SCAN team at CMH. Five children were excluded from the study as 3 died and 2 were transferred to another hospital. The number of patients with < 50% of follow-up needs addressed was reduced from 47% to 43%. All follow-up needs were addressed in 13% (3/23) of patients. Conclusions: While project aims weren’t met, there was progress. Next steps include educating all discharging teams at CMH as there is no single team discharging these patients. Overall, there are few of these patients so standardization of discharge practices is challenging. SCAN created a working group and point person for appointment tracking to ensure follow-up needs established at discharge.
-

A Rare Case Of Adolescent Epiglottitis Secondary To Streptococcus Dysgalactiae
Kedar Tilak, Mohamed Aashiq Abdul Ghayum, Douglas Swanson, and Rana El Feghaly
Streptococcus dysgalactiae causes pharyngitis, cellulitis, necrotizing soft tissue infections, sepsis, and streptococcal toxic shock syndrome • It can lead to both toxin-mediated and immune-mediated diseases • Mostly seen in adults, rare in pediatric patients • Here we present a 15-year-old with S. dysgalactiae- associated septicemia, and epiglottitis with extensive neck infection
-

Bisphosphonate Treatment in Pediatric Patients with Rare Ovarian Malignancy and Hypercalcemia: A Case Series
Seth Lamb, Samhita Bhattarai, and Jennifer Boyd
Objective: To describe the presentation, management, and outcomes of severe hypercalcemia in two adolescent females secondary to ovarian malignancy. Methods: The case series includes two adolescent female patients, aged 11 and 16, diagnosed with rare ovarian malignancies and associated hypercalcemia. The 11-year-old female was diagnosed with small cell carcinoma of ovary while the 16-year-old was diagnosed with dysgerminoma. Both patients presented with abdominal pain, nausea and constipation. The 11-year-old received zoledronic acid while the 16-year-old received pamidronate. Serum calcium level, symptoms and adverse effects were monitored before and after both medications. Results: Both patients presented with severe hypercalcemia. The 11-year old presented with serum calcium of 15.0 mg/dL while the 16-year old presented with a serum calcium of 15.9 mg/dL. Both patients were refractory to hyperhydration with isotonic normal saline and 3 or more doses of calcitonin over a span of 3 days. Patients were then given bisphosphonates to decrease severe hypercalcemia. Patient 1 received one dose of zoledronic acid 0.1 Unit/kg while patient 2 received pamidronate. Calcium decreased to 10.4 mg/dl in 56 hours after zoledronic acid administration. Patient also had her tumor resection 3 days after medication administration which further decreased serum calcium to a lowest of 6.9 mg/dl. This was improved after 1 dose of intravenous calcium gluconate. Patient 2 received 1 dose of pamidronate 0.37 mg/kg. Serum calcium decreased to 9.1 mg/dl in 41 hours. Patient had surgical debulking surgery the same day. Lowest post operative calcium level for patient 2 was 7.5 mg/dl 3 days post pamidronate and 1 day post tumor debulking. Diagnosis was confirmed by pathology to be small cell carcinoma of ovary-hypercalcemia type and dysgerminoma respectively for patient 1 and 2. Patient 1 required calcium supplementation for 5 days post-surgery while patient 2 needed no calcium supplementation. No adverse effects noted on both patients. Conclusion: Small cell carcinoma of ovary and dysgerminoma are rare causes of hypercalcemia in adolescents. These cases highlight the importance of recognizing paraneoplastic hypercalcemia, safety, efficacy, and monitoring for hypocalcemia after a single dose of bisphosphonate. Close monitoring is needed if patients plan to undergo tumor resection within the next week as both medications are known to have a long half-life.
-

Dental Considerations for a Pediatric Patient with Osteopetrosis: Case Report
Bethany Castro, Robin Onikul, Neena Patel, Jenna Sparks, Amy Burleson, and Brenda S Bohaty
Introduction: Osteopetrosis is comprised of a group of rare hereditary disorders characterized by impaired osteoclast development or activity resulting in altered bone metabolism and high bone mineral density. Resulting bone is denser and heavier but more fragile than healthy bone. This condition can have oral manifestations such as malformed teeth, hypomineralization, or agenesis of teeth. The treatment for osteopetrosis can include hematopoietic stem cell transplantation and recommendations for prophylactic dental treatment7. The purpose of this report is to present a review of the literature regarding the dental considerations for patients with osteopetrosis. Case Report: This case report details a six-year-old male who initially presented to the Children’s Mercy Dental Clinic in 2020 for dental clearance prior to a bone marrow transplant and the subsequent follow up care over the next four years. The patient’s medical history is significant for osteopetrosis status post bone marrow transplant in 2020 as well as numerous medical diagnoses. Clinical and radiographic examination revealed carious primary teeth and multiple malformed, hypoplastic, or unerupted successor teeth. Clinical considerations for this patient include managing carious teeth as well as providing the parent with recommendations regarding future care are presented in this report.
-

Differential Diagnosis of Oral Ulcerations: a Case Report
Richard Nguyen, Kaitlin Carlson, Meredith Clark, Amy Burleson, Brenda S Bohaty, Robin Onikul, Neena Patel, and Jenna Sparks
The diagnosis of oral lesions in children can be challenging as it can be an unspecified symptom of several diseases. Differential diagnoses can range from infectious diseases of childhood, inflammations, nutritional deficiencies, and chronic diseases. Because of this, children with oral ulcers may be treated by different specialists such as pediatric dentists and pediatricians. The purpose of this poster is to report the case of a twenty-one-month-old female patient who presented to Children’s Mercy Hospital Kansas City Emergency Department with chief concern for acute onset of intraoral oral ulcers, extraoral blisters near the lower lip, and fetid oral odor. Patient has a complex contributory medical history. This poster presents a review of the literature regarding various diseases associated with oral ulcers along with the potential development of acute necrotizing ulcerative gingivitis
-
Increasing incentive spirometry use in patients with sickle cell disease admitted to CMH
Juan Nario Ramirez, Alexandra Prosser-Dombrowski, Thomas R. Cochran, and Joel Thompson
Acute chest syndrome is one of the leading causes of morbidity and mortality in patients with sickle cell disease. The National Heart, Lung, and Blood Institute (NHLBI) recommends that patients with sickle cell disease perform ten breaths of incentive spirometry (IS) every two hours while awake to prevent development of acute chest syndrome. By not meeting these guidelines, patients are more likely to develop this potentially life-threatening acute complication. To increase the use of IS in patients with sickle cell disease admitted to the hospital for vaso-occlusive pain. Patients were identified and IS occurrences were measured via review of electronic medical record. Of those patients admitted with sickle cell vaso-occlusive pain, the frequency that IS was offered or performed each hospital day was recorded. Partial admission and discharge days were excluded. For PDSA cycle 1, all IS orders in Cerner powerplans were updated to reflect current NHLBI recommendations. Additionally, education was provided to residents and nursing staff regarding the importance of the use of IS to prevent severe complications such as acute chest syndrome. Following PDSA cycle 1, a second meeting with stakeholders led to changing IS documentation to coincide with the required task of patient-controlled analgesia (PCA) assessment every two hours. Furthermore, as it is difficult for younger children to use IS appropriately, a new PCA form was created to document the use of alternatives to IS such as pinwheels or bubbles. Data obtained from 10/2023-12/2023 and 10/2024-12/2024 was then reviewed to evaluate the impact of PDSA cycle 2. From 8/2021-11/2021, there were 191 hospital days with patients admitted with sickle cell vaso-occlusive pain, of which 53% had IS documented. When IS was documented, 0% of patients received the recommended frequency of IS and the median hours between IS occurrences was 6.3 hours. From 12/2021-3/2022, 164 hospital days had IS documented 40% of the time with 2% of hospital days meeting the recommended frequency and 5.9 median hours between IS occurrences. From 8/2022-11/2022, 167 hospital days had IS documented 26% of the time with 12% of hospital days meeting the recommended frequency and 3.0 median hours between IS occurrences. From 10/2023 - 12/2023, 181 hospital days had IS documented 12.7% of the time with 9% of hospital days meeting the recommended frequency and 5.6 median hours between IS occurrences. From 10/2024 - 12/2024, 177 hospital days had IS documented 11% of the time with 15.7% of hospital days meeting the recommended frequency and 4.1 hours between IS occurrences. Implementation of uniform IS orders that match NHLBI recommendations resulted in an increase in the provision and frequency of IS used among the studied population. In PDSA cycle 2, implementation of IS documentation along with analgesia assessments resulted in an overall improvement of the median hours between IS occurrences and the number of hospital days with IS given at the recommended frequency, when IS was documented. It is important to note that the overall number of times in which IS was documented decreased compared to the first two cycles, however, the percentage of patients using IS at the recommended frequency continued to improve. For the next PDSA cycle, we will plan to address other potential barriers to IS documentation, such as accessibility to IS in the Hematology/Oncology inpatient unit . Further research will also focus on evaluating the impact of appropriate use of IS on the development of acute chest syndrome in our patient population.
-

Oral Surgical Needs in a Pediatric Hospital Dental Clinic
Meredith Clark, Richard Nguyen, Kaitlin Carlson, Brenda S Bohaty, Amy Burleson, Robin Onikul, Neena Patel, and Jenna Sparks
Purpose: The aim of this study is to evaluate and assess the oral surgery needs in a pediatric hospital dental clinic at Children’s Mercy Hospital in Kansas City. Methods: Following IRB approval, appointments over a 6-month time-period were reviewed and recorded when a referral was placed to an oral surgeon. The reason for referral, patient age and medical history were recorded and analyzed. Results: Half of the patients needing oral and maxillofacial procedures were between the ages of 8-10 years old. There was an equal number of patients needing extractions due to carious/non-restorable teeth with and without special health care needs. Two-thirds of the patients were referred from an outside provider to Children’s Mercy Hospital. Conclusion: Due to the oral surgery needs of patients that are seen in the Children’s Mercy dental clinic, it would be beneficial to the patient population to have an oral surgeon on staff. This would provide better access to care by eliminating barriers in the referral process and reducing time to treatment completion.
-

Physician Use of Progesterone in transgender adolescents: A survey
Samhita Bhattarai and Michelle Knoll
Objectives To evaluate the current perspective and clinical practices of physicians regarding the use of synthetic progestins as an adjunct to estrogen therapy in transfeminine adolescents. The survey focuses on perceived benefits, risks and overall efficacy in gender affirming hormone therapy. Methods A cross sectional survey was conducted among physicians who care for transfeminine patients. The survey included questions regarding their specialty, practice setting, age range of patients. Data was also collected regarding their indication for use, perceived benefits (e.g. breast development) and rationale if not using progestins for this purpose. Results Of 110 physicians who participated in the survey, 85 (77.2%) endorsed providing gender affirming care. Of those 85 respondents, 71(83.5%) have used progestins in some way, and 57 (67%) have used them as an adjunct to estrogen. Other uses included for contraception or amenorrhea in transmasculine patients, for suppression of endogenous puberty, and to induce patient requested hormone cycling. The most common form of progesterone used was oral progestin at 80.2% while depo medroxyprogesterone was used 21.1% Majority of the physicians (46/57, 80.7%) responded to being either somewhat satisfied or neutral to use of progestins. Of those who do not use progestins in transfeminine patients, most respondents noted lack of data on efficacy and side effects or lack of recommendations in guidelines. Others noted that it has not been necessary in achieving desired outcomes. Conclusions The survey indicates that while a significant number of physicians who practice gender affirming care incorporate progestins into hormone therapy for transgender youth, there was interest in more data on benefits and side effects on their use in transfeminine patients. Further research is needed to add to the current WPATH guideline to ensure more patient centric care along with ensuring its safety and effectiveness.
-

Primary Molar Loss and Resulting Space Outcomes: a Systematic Review
Kaitlin Carlson, Meredith Clark, Richard Nguyen, Brenda S Bohaty, Amy Burleson, Robin Onikul, Neena Patel, and Jenna Sparks
Premature loss of a primary molar can occur due to a multitude of reasons, including caries, infection, and trauma. When this occurs and restoration of the affected primary tooth is not possible, the AAPD recognizes space maintenance as a “Best Practice” to prevent loss of arch length, width, and perimeter after extraction. However, reports suggest that with proper intercuspation of first permanent molars, space loss from premature loss of a primary molar is minimal and a space maintainer in that area may not be needed. The clinical management for such cases has been controversial across pediatric dental providers, with factors such as timing, behavior, and age all playing large roles in making treatment planning complex. This systematic review is aimed at reviewing the current scientific literature to evaluate the need for a unilateral space maintainer after premature loss of a primary molar in the mixed dentition stage. For sake of completion, studies that looked at loss of first primary molars and/or second primary molars were included. Bilateral space maintenance, such as lower lingual holding arches or Nance appliances, is not investigated in this review due to its relative effectiveness across clinical cases. A systematic review is needed to help guide clinicians’ decision making and provide clarity for management in the currently ambiguous scenario of the premature loss of a primary molar in the mixed dentition stage.
-

Acceptability of a Brief Acceptance and Commitment Therapy Intervention for Caregivers of Children with Pediatric Feeding Disorder
Emma Murray, Taylor P. Harris, Annie L. Ryder, Alexandra Zax, Taylor M. Datillo, Corey Schurman, Laura Slosky, Sarah T. Edwards, Delwyn Catley, Ann M. Davis, and Dana Bakula
Introduction: Pediatric feeding disorder (PFD) affects 1 in 37 young children and is associated with heightened stress and anxiety among caregivers. Currently, there are no established interventions that target PFD caregiver stress, and traditional models of adult mental healthcare face feasibility issues in pediatric care settings. To address this gap, we developed a brief acceptance and commitment therapy (ACT) intervention (Clinical Trials #NCT06001398). We assessed caregiver-perceived acceptability to inform future efficacy testing. Method: Twenty caregivers participated in a NIMH-funded pilot study of a 2-session ACT intervention for parents of children with PFD. Caregivers with children aged 2 to 6 years with PFD were recruited and randomized to either the active (n = 14) or control intervention (n = 6). Intervention content included psychoeducation, ACT skills training, and application of ACT skills to mealtimes. Caregivers’ rated intervention acceptability at 3-month follow-up. Results: Eight caregivers who received the ACT intervention completed acceptability measures. Most (75%) found it “somewhat” or “very” helpful. 62% reported using the ACT strategies 3 months following intervention completion and 88% said they would recommend this program to other parents. Most (88%) reported the same level of confidence in managing their own stress as prior to the intervention. Descriptively, caregivers enjoyed the sessions (“I enjoyed the sessions and just being more mindful of how my own stress was impact[ing] our mealtimes”). Conclusions: Caregivers found this brief ACT intervention to be highly acceptable. Caregivers reported regular use of the strategies, positive perceptions of the program, and that they would recommend it to others. Interestingly, they did not report feeling that their confidence in managing their stress improved. It is possible that retrospective comparisons about stress management may be difficult to assess, making it critical that we complete rigorous efficacy testing with pre-post measures of stress. Further efficacy testing is needed.
-

AHT Diagnoses: The Influences of Clinical Presentation and Evidence of Impact
Ruairi Smith-Dewey, Angela Bachim, Colleen Bressler, Kristine Campbell, Lori Frasier, Christopher Greeley, Danielle Horton, Nicole Johnson, Jan Leonard, Megan Letson, Caitlin McNamara, Ashley K. Sherman, Shalon Nienow, Joanne Wood, and James Anderst
In cases where Child Abuse Pediatricians (CAPs) diagnose abusive head trauma (AHT) in young children, some factors surrounding the diagnosis have been challenged including causative shaking, necessity of external signs of impact, or concomitant suspicious injuries. Evaluation of CAP diagnoses in children with subdural hemorrhage (SDH) can give insight into factors related to the frequency of abusive head trauma (AHT) diagnoses. Additionally, characterization of those with SDH+CSI without evidence of impact may inform controversies around AHT diagnoses. Objective We aim to compare CAP diagnoses in subjects with SDH across clinical presentations and in the context of evidence of head impact. We also aim to describe the subjects with SDH+CSI and no external signs of impact to the head. Design/Methods Retrospective case-control study using Child Abuse Pediatrics Research Network (CAPNET) data from 10 sites over 27 months. Subjects were < 24 months old with SDH and in-person CAP evaluation. Subjects were divided into groups based on study determined criteria: Ill SDH only, Non-ill SDH only, and SDH with CSI. Ill status was categorized by clinical signs of cardio-respiratory collapse and/or significantly altered consciousness. CSIs are injuries highly associated with abuse in the following categories: skin, bones, eyes, and abdomen. CAP diagnosis of abuse was defined as 5-7 on a 7-point scale. Abuse diagnoses were compared across study groups. Head impact signs included bruising to the head, scalp swelling, and skull fractures. Comparisons used unadjusted odds ratios with 95% confidence intervals. Results Of the 492 study subjects, 386 (78%) were diagnosed with AHT. The SDH+CSI subjects were more likely to be diagnosed with abuse than Ill-SDH (OR 2.7, 95% CI 1.3-5.6) and Non-ill SDH (OR 7.2, 95% CI 4.3-12.1). Of the 276 subjects without signs of head impact, 215 (78%) were diagnosed with abuse. In this subgroup, SDH+CSI were more likely to be diagnosed with abuse than Ill-SDH (OR 3.7, 95% CI 1.5-9.2) and Non-ill SDH (10.3, 95% CI 5.0-21.1). Of the 157 subjects with SDH+CSI and no signs of head impact, 88/157 (56%) had non-head/eye related CSIs, including 52/88 (59%) with high specificity fractures and/or multiple fractures, 48/88 (55%) with high specificity bruising. Multiple types of CSIs were in 22/88 (25%). Conclusion(s) Among children with SDH, AHT is more frequently diagnosed in the presence of CSIs, particularly in the absence of external signs of impact. The high prevalence of CSIs in cases with SDH and no external signs of impact indicates that AHT can occur absent external signs of head impact.
-

A Risk Score to Predict Recurrent High Intensity Inpatient Resource Utilization for Children with Medical Complexity.
Charles Maloy, Matt Hall, Jessica L. Bettenhausen, YR Chan, Leah Jones, Kathryn Kyler, Laura Plencner, Jessica Markham, Jacqueline Walker, Smit Shah, Sian Best, Jonathan Ermer, Shelby Chesbro, Maria Newmaster, and Hank Puls
Background
Children with medical complexity (CMC) use a greater amount of inpatient resources and stand to benefit from unique care models and coordination. However, hospital resources can be limited, and a better understanding of which CMC are high resource users could improve hospital and staff planning.
Objective:
To develop a risk score predictive of recurrent high intensity inpatient utilization among CMC.
Methods:
We conducted a retrospective cohort study of children < 18 years old with ≥3 complex chronic conditions (CCC) discharged from one of 48 children’s hospitals in the Pediatric Health Information System during 2021 and 2022. To reflect CMC typically cared for by a general medical service, children with cardiac procedures, dialysis, oncology, or transplant CCCs, and index hospitalization mortality were excluded. We used multivariable logistic regression to determine factors present on the index hospitalization associated with ≥5 hospitalizations or ≥3 hospitalizations with one lasting ≥25 days within any 365-day period (high inpatient utilization) in 2021-2023. We developed risk scoring system using model coefficients and defined the optimal risk score cutoff to maximize sensitivity and specificity. We then applied the risk score cutoff to children discharged to determine (a) ratio of predicted:actual CMC with recurrent high resource use and (b) the total predicted daily volume on 50th, 75th, and 90th percentile days for each hospital.
Results:
Of 44,432 included children , 9,596 (21.6%) had high inpatient utilization (Table). Children under 1 year of age had the highest odds of high inpatient utilization (OR 2.26 [95% CI: 2.16, 2.37]) and all CCC and technology groups (except metabolic) met statistical significance (Figure 1). The optimal risk score cutoff was 29 and predicted 17,411 (39.2%) CMC as high inpatient resource utilizers; the predicted: actual ratio of CMC with high inpatient utilization was 1.81. The mean daily census of the 50th, 75th, and 90th percentiles across hospitals was 28 CMC with recurrent high utilization (± 17), 34 (±18), and 39 (±19; Figure2).
Conclusions:
It is feasible to develop a risk score predictive of recurrent high inpatient utilization among CMC. There is substantial variability in volume of CMC with high utilization between pediatric hospitals. The risk score cutoff values can be modified to suit different applications and institution-specific objectives. These applications could include a dedicated service line or staffing. Alternatively, this could identify patients who would benefit from more formal handoff from inpatient to outpatient providers.
-
Decreasing time to narcotic pain medication in patients with sickle cell disease presenting with acute pain crises in a pediatric emergency department: a quality improvement initiative
Allison Adam, Lina Patel, Christopher Kaberline, Ibad Siddiqi, and Leslie Hueschen
-

Facilitators, Barriers, & Recommendations for Pediatric Research Sites Conducting Decentralized Clinical Trials (DCTs)
Abby Kietzman
The COVID-19 pandemic drastically altered the way clinical research is conducted through a widespread adoption of telemedicine practices to continue clinical trial procedures during peak periods of global COVID-19 spread. Using telehealth/telemedicine services allows researchers to conduct “decentralized clinical trials”, or DCTs, for all or portions of study protocol procedures while maintaining safety measures implemented for pandemic control. However, research sites are hesitant to adopt DCT policies due to concerns around digital health technology, data safety and quality, and limited information in the literature specifically assessing telemedicine use for pediatric clinical research via DCTs or how equipped pediatric research sites are for the transition away from the site. A cross-sectional, observational casestudy surveying clinical research professionals (CRPs) at a local pediatric institution in Kansas City, MO, was conducted to better understand pediatric site facilitators and barriers to implementation and utilization of DCTs from a site perspective.
-

In Search of the Unknown Mimic of Abusive Head Trauma (AHT)
Ruairi Smith-Dewey, Angela Bachim, Colleen Bressler, Kristine Campbell, Lori Frasier, Danielle Horton, Nicole Johnson, Jan Leonard, Megan Letson, Caitlin McNamara, Shalon Nienow, Ashley K. Sherman, Stuart Sommers, Joanne Wood, and James Anderst
Background Child Abuse Pediatricians (CAPs) are accused of misdiagnosing a yet-to-be-identified mimic as abusive head trauma (AHT), particularly in ill children with an isolated subdural hemorrhage (SDH). Though not diagnostic criteria, specific social stressors are identified as AHT risk factors. The existence of a mimic can be assessed by comparing the prevalence of AHT risk factors across study groups (See Table 1). Objective We hypothesize that the distribution of AHT risk factors will be: fewer in the CAP-identified mimic group versus the CAP-diagnosed abuse group, no difference between ill SDH only and SDH+CSI groups as these are likely the same condition, and fewer in the non-ill SDH only versus SDH+CSI groups as there are likely undocumented known mimics in the non-ill SDH only group. Design/Methods Retrospective case-control study using Child Abuse Pediatrics Research Network (CAPNET) data from 10 sites over 27 months. As proof of concept, the prevalence of AHT risk factors was compared between CAP identified mimics and CAP-diagnosed abuse groups. Social risks were compared using unadjusted odds ratios with 95% confidence intervals. For social risk comparison across SDH groups, subjects were < 24 months old and evaluated by a CAP. Ill subjects had cardio-respiratory collapse and/or significantly altered consciousness. CSIs were injuries that are highly associated with abuse in the skin, bones, eyes, and abdomen. CAP diagnosis was not considered for SDH group determination. Prevalence of social risk, demographics, and trauma history were compared between groups using two one-sided equivalence tests with a 20% equivalence margin. Results In proof of concept, 1058 subjects with known medical mimics had statistically significantly fewer AHT social risk factors than 548 abused subjects with ICH/fracture in 5/7 domains. In the main study, when comparing the 350 SDH+CSI subjects and 46 Ill SDH subjects, the two groups were statistically equivalent in 5/7 social risks. When comparing the 350 SDH+CSI and 96 Non-Ill SDH subjects, they were statistically equivalent in 2/7 social risks. Provision of trauma history was equivalent across all three groups (RD –0.01-0.10). Conclusion(s) Social risk distribution differentiates CAPNET subjects with medical mimics from those without. Social risk distribution largely did not differ between SDH+CSI and Ill-SDH groups, indicating that a yet-to-be-identified mimic is not widely prevalent in the Ill-SDH group. Non-ill appearing subjects with SDH appear to have fewer AHT risks compared to SDH+CSI, supporting possible medical causes in some of these children.
-
Maternal Guilt Following Pediatric Burn Injury
Sabrina Ung, Abby Dugan, Casey Lawless, Mallory Netz, Alec Bernstein, and Carisa Parrish
Background: Previous research has shown that parental guilt is a risk factor for poor parental adjustment (e.g., depression, posttraumatic stress) following a pediatric burn injury (Hawkins et al., 2019). However, few studies have examined risk factors for parental guilt. Objectives/Goal: The current study aimed to examine relationships among demographic variables, burn characteristics, maternal mental health, with maternal guilt following their child’s burn injury. Methods/Design: Mothers of 147 children who experienced a burn injury (mean child age = 6.28 years, 46% female, 44.7% White, 19.2% Black or African American, 9.6% Hispanic, 1.3% Asian, 11.9% multiracial, total body surface area range .10 – 15%) were screened using questionnaires assessing parent posttraumatic stress, depression, anxiety, and guilt during their children’s outpatient burn clinic visit. Clinical and demographic variables were retrieved retrospectively from patients’ medical charts. Descriptive statistics and linear regression analyses were conducted. Several demographic factors (e.g., child’s sex, race, insurance type) and burn injury characteristics (e.g., length of hospital stay, burn injury mechanism) were found to be nonsignificant in bivariate correlational and regression analyses and therefore were excluded in final analyses. Results: Maternal depressive symptoms (β = .23, p = .04) and posttraumatic stress related to their child’s burn injuries (β = .49, p = < .001) significantly predicted maternal guilt. Mothers of younger children were observed to experience higher levels of guilt (β = -.15, p = .03). Lastly, burn size (β = -.11, p = .14) and maternal anxiety (β = .00, p = .99) were not significant predictors of maternal guilt. Conclusions: Following a burn injury, maternal posttraumatic stress, depressive symptoms, and child age contribute to maternal guilt related to the injury regardless of burn size. Findings support integration of routine screening of caregivers’ guilt and mental health following pediatric burn injuries, regardless of burn size, to inform appropriate interventions.
-

Opportunities for Solid Organ Donation in the Neonatal Intensive Care Unit
Sarah Pippin, Ashley Sherman, Julie Weiner, and Jotishna Sharma
Background: Pediatric patients are at an increased risk of mortality when waiting for an organ transplant. Approximately 50% of pediatric patients wait for> a year for a solid organ transplant and infants < 1 year of age have the highest death rate while awaiting transplantation. There are two pathways for organ donation (OD), donation after death by neurologic criteria (DDNC) or donation after circulatory determination of death (DCDD). Neonates rarely meet brain death criteria, and since most deaths in the NICU occur aftera planned extubation, DCDD with organ procurement after a planned extubation from mechanical ventilation can be a consideration especially with kidney and liver donations. Organ procurement may be limited by warm ischernic time (WI1); usually :'.S 90 minutes. The question remains which neonates would meet criteria for DCDD.
Purpose: The aim of this study is to characterize theoretical eligibility of DCDD in infants undergoing withdrawal of care in the NICU based on WIT :'.S 90 minutes
Method: Retrospective study of a cohort of infants 2:36 weeks at the time of death who died at a level IV NICU from January 1, 2012, to December 31, 2022. Demographic information was obtained. Mode of death was categorized as withdrawal of care, withholding of care, or CPR. The withdrawal of care was further examined for eligibility for DCDD based on WIT :'.S 90 minutes.
Results: During the study period, there were 337 infants 2': 36 weeks at the time of death and of those, 67% (226/337) infants had withdrawal of care. The most co=on cause of death was congenital anomalies. Those who met DCDD criteria were found to have significantly higher birth weight (p=< 0.01), older GA at birth (p=0.01), and older PMA at death (p=
Conclusion: One third ofNICU deaths 2::36 weeks undergoing withdrawal of mechanical ventilation could be potential solid organ donor after DCDD with WIT ::S 90 minutes. Increased organ donation opportunities in this age group could have an impact for pediatric patients waiting for an organ transplant. Establishing a DCDD protocol in level IV NICUs should be strongly considered. Further studies are needed to determine factors that predict success of neonatal solid organ donation through DCDD.
-

Reducing Antibiotic Duration for Pneumonia and Sinusitis in the Emergency Department: A Quality Improvement Approach
Joshua Saucedo, Leslie Hueschen, Amanda Nedved, Marsha Dannenberg, Patricia Phillips, Jennifer Floyd, Alaina N. Burns, and Rana El Feghaly
Background: Antibiotic duration is one of the pillars of antimicrobial stewardship programs (ASP) as it helps to limit unnecessary antibiotic exposure while continuing to provide appropriate care for infections. In our emergency department (ED), clinicians are using first-line guideline-recommended antibiotics as an appropriate choice for most patients (per our ASP report tracking), however, duration continues to be prolonged especially for community acquired pneumonia (CAP) and acute bacterial rhinosinusitis (ABRS). National guidelines recommend shortening antibiotic durations to 3-5 days for CAP and 5-7 days for ABRS, however currently only 22% of patients discharged from our ED receive the recommended duration. Objective: Our aim is to increase percentage of children discharged home from the ED with a diagnosis of CAP or ABRS treated with an optimal antibiotic duration (5 days or less for CAP, 7 days or less for ABRS) from 22% to 70% by July 2025, while assessing for differences in care based on demographic and socioeconomic factors. Design/Methods: A multidisciplinary team (infectious diseases physicians, ED and urgent care physicians, advanced practice providers, nurses, and pharmacy) formed in December 2023. Outcome metric is the percentage of patients receiving recommended antibiotic duration for CAP or ABRS; data trends analyzed monthly and process changes implemented according to the SPC Out of Control Process Western Electric rule set. Process metrics include use of order set, quick discharge order set, and QR code. Balancing metric is the number of return visits with the same discharge diagnosis within 14 days. Utilizing cause-and-effect diagram, driver diagram (Figure 1), and PICK chart (Figure 2), we identified possible interventions. Plan-Do-Study-Act cycles so far have included implementation of new internal CAP, updates to electronic medical record and quick discharge order sets. A survey of prescriber comfort with shorter duration identified barriers and provided education, which has led to posting evidence for lower duration treatment to prescribers in their workrooms and developing new ABRS CPG. Results: We have shifts in the central line of our overall outcome in August 2023, May and July 2024 to 65.4% with no change in balancing metric (Figures 3A-CQBS, annotated with PDSA cycles). Discussion: We have seen a reduction in the duration of antibiotics for CAP and ABRS with electronic medical record and prescriber education interventions. Future cycles will focus on barrier mitigation and increased data transparency, with huddle board reminders and positive encouragement to providers.
-
Reducing Vancomycin in a CICU
Karoline Krzywda, Lauren Johnson, and Allison Taber
Introduction: In the cardiac intensive care unit (CICU) empiric vancomycin is frequently prescribed. This practice occurs without wide knowledge of the true rates of methicillin resistant staph aureus (MRSA) and methicillin resistant staph epidermidis (MRSE) infections. Given the potential for harmful side effects of vancomycin as well as concern for growing antibiotic resistance we sought to better characterize local unit prescribing practices and MRSA/MRSE infection rates to guide our quality improvement project with an aim of reducing vancomycin use in our CICU. Methods: This project is taking place at Children’s Mercy Kansas City CICU, a 24 bed unit with an average of 274 pump cases per year. Patient data from January 2021-January 2023 was analyzed. There were approximately 20-60 vancomycin days per month with a center line of 0.1, indicating that over that time frame, 10% of the patient days were vancomycin days. In 2021 there were 111 orders for Vancomycin. Using a Pareto chart, we found that a majority (52) of Vancomycin orders were for fever alone. We analyzed all positive cultures in 2021 and of the 111 vancomycin orders there were only 11 positive MRSA/MRSE infections for which Vancomycin was prescribed as a full treatment course. We aim to reduce the number of vancomycin days from 0.1 per 1000 patient days to 0.075 per 1000 patient days by May 2025. Given the mismatch between prescribing habits and true infection rates, our first test of change will be to provide education regarding MRSA/MRSE infection rates in the CICU and current prescribing habits. Additionally, we will ask that providers not order vancomycin if a patient has a fever alone without hemodynamic instability, without high or increasing inflammatory markers, has not had a heart transplant, is not on extracorporeal membrane support or a ventricular assist device or is not immunocompromised. As a balancing measure we will track MRSA/MRSE positive cultures that did not receive vancomycin prior to culture results. Results: Insufficient time has passed to evaluate the project’s first test of change. Conclusions: Vancomycin is frequently empirically prescribed with low rates of MRSA/MRSE infections in our CICU. Our first test of change is to provide education on rates of MRSA/MRSE infections and vancomycin prescribing habits in our CICU. We will be monitoring for decrease in the number of vancomycin days as well MRSA/MRSE infections in which empiric therapy with vancomycin was missed.
-

Detection of Chromosomal Mosaicism- the Importance of Karyotyping and FISH
Allison Kalinousky, Jennifer Roberts, Madeeha Alikhan, John Herriges, Lei Zhang, and Elena Repnikova
Introduction: The use of whole-exome/whole-genome sequencing for the detection of sequence-level variants and copy number variations (CNV) is increasingly being adopted as a primary testing method for genetic disease diagnosis by many institutions. Additionally, long-read sequencing is a promising technique to capture not only sequence level variants and CNVs but also structural chromosomal abnormalities. Significant progress has been achieved in this field; however, the detection of chromosomal mosaicism, including numerical gains and losses, rings, markers, and structural rearrangements – particularly those that are lineage-specific or exist at low levels – might still pose challenges with these emerging technologies. Furthermore, differentiating various mosaic cell lines may not be feasible. Literature review shows that chromosomal mosaicism is estimated to occur in up to 70% of human preimplantation embryos. Clinically significant chromosomal mosaicism is reported in ~3% of products of conceptions (POC), 1-2% of chorionic villus sampling (CVS), 0.1-0.3% of amniotic fluids (AF) samples, and 0.05-0.1% postnatal samples when assessed using conventional cytogenetic methods. To date, there are no studies available that provide data on the accuracy and detection levels of chromosomal mosaicism using third of fourth generation sequencing technologies. Methods: We conducted a retrospective review of patients who underwent conventional cytogenetic testing (chromosome analysis via Giemsa staining and fluorescence in situ hybridization (FISH)) for various clinical indications at Children’s Mercy Hospital from 2003 and 2023. Within this period, we received 20,866 constitutional cases of with 4,414 were cytogenetically abnormal. We also evaluated 762 cases submitted for exome sequencing with copy number analysis in 2023. We then examined all mosaic cases. Results: We found that the average number of mosaic cases each year was 29 (range: 9-39), accounting for ~3.1% of all clinical cases studied and ~14% of all abnormal cases per year. Levels of mosaicism were variable, ranging from 4 to 95%. Of all cases (both normal and abnormal) across all years, 4.7% of POCs, 4.3% of AF samples, and 2.7% of peripheral blood (PB) samples had chromosomal mosaicism. In comparison to the 762 PB exome cases, only three were mosaic (two with trisomy 9 and a ring(X)) totaling ~0.4% of postnatal cases. Numerical abnormalities are the most common form of mosaicism in our cohort, accounting for ~79% of mosaic cases. Of the numerical abnormalities, sex chromosomes are the most frequently implicated, with an average involvement of 44% in POCs, 40% in AF samples, and 79% in PB. The most common numerical abnormality of the autosomes in POCs were affecting chromosomes 22 (7%), 15 (6%), and 16 (5%); in AF samples affecting chromosomes 21 (20%), 18 (7.5%), and 22 (5%); and in PBs affecting chromosomes 21 (11%) and 18 (4%). Approximately 14% of mosaic cases harbored a structural abnormality of the autosomes. The most common abnormality in PBs involved the Y chromosome (12%), and in POCs involved chromosome 13 (19%). The structural abnormalities in AF samples affected chromosomes 3, 7, 9, 12, 14, 16, 18, and 22 at relatively equal prevalence. Discussion: Review of our data indicates a higher prevalence of chromosomal mosaicism identified through conventional cytogenetic methods across various specimen types compared to existing literature. Furthermore, our limited genomic sequencing data suggests that conventional cytogenetic technologies may detect chromosomal mosaicism more frequently than genomic technologies. These findings underscore the importance of employing karyotyping and FISH for the detection of chromosomal mosaicism, particularly at low levels, which may be missed by genomic sequencing. Additionally, a thorough examination of clinical phenotypes can enhance the suspicion of mosaicism, ultimately enhancing diagnostic rates.
-

Development of Mobility Scales for Infants and Children on ECMO
Johanna I. Orrick, Debra E. Newton, and Caroline Holton
Extracorporeal Membrane Oxygenation (ECMO) is a life-saving intervention commonly used in pediatric and neonatal intensive care; however, it presents unique challenges for maintaining patient mobility. Early mobility contributes to better long-term outcomes. Existing mobility scales by the Extracorporeal Life Support Organization (ELSO) are limited to patients aged 8 years and older, leaving a gap for younger populations. This study aimed to develop and validate mobility scales specifically for infants (< 2 years) and children aged 2-8 years undergoing ECMO therapy. Through a collaborative effort involving pediatric ECMO specialists, physicians, and critical care nurses, we adapted ELSO’s mobility criteria to be developmentally appropriate for these younger age groups. For infants, mobility benchmarks include passive and active limb movements, head control, and supported sitting. The criteria for children aged 2-8 is expanded to include sitting, supported standing, and age-appropriate gross motor activities. This scale provides graded levels of mobility that accommodate ECMO-specific safety considerations, allowing practitioners to chart interventions according to each child’s developmental and physiological capacity. The resulting scales are being pilot-tested at our large ECMO center, with data showing preliminary effectiveness at capturing the degree of mobility achieved during ECMO runs. This mobility scale fills a critical need by providing structured charting guidelines for mobilizing infants and young children on ECMO, promoting functional recovery and potential improvements in long-term developmental outcomes. Further studies are recommended to establish consistency across institutions and confirm the scale's impact on mobility outcomes in pediatric ECMO patients.
-
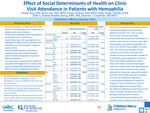
Effect of Social Determinants of Health on Clinic Visit Attendance in Patients with Hemophilia
Shailly Gaur; Brian Lee PhD, MPH; James Anderst MD, MSCI; Katie Foote LSCSW, LCSW, OSW-C; Andrea Bradley-Ewing MPA, MA; and Shannon L. Carpenter
Background Social determinants of health (SDOH) create barriers to seeking care regularly, especially for patients with chronic disease. Patients with moderate-severe hemophilia A and B (factor 8 and 9 deficiencies respectively) have a life-long higher risk of bleeding and require chronic therapies. Specialized care is offered through hemophilia treatment centers (HTCs); however, these can be difficult to access for some individuals. Previous SDOH research in this patient population has been limited; therefore, it can be difficult to identify the barriers to care that exist. There is a need to examine SDOH more thoroughly to create patient-directed interventions to improve access to care. Objectives To identify common SDOH affecting patients with moderate-severe hemophilia and determine how each impacts clinical utilization within a single HTC. Methods A retrospective chart review of patients age < 18 years old with a diagnosis of moderate or severe hemophilia A or B seen at Children’s Mercy Hemophilia Treatment Center over the last five years. Dependent variables included no-show visits, which were any missed visit since the patient established care, and missed yearly comprehensive visits, of which non-parametric distributions were calculated. Rates were standardized to an assumed 10-year follow-up period and then compared across independent variables including race, ethnicity, language spoken, insurance type, rural vs urban home, food insecurity rate, poverty level, distance to an ER and to the HTC using the Kruskal-Wallis and Wilcoxon rank-sum tests, where appropriate. Significant findings were determined using a p-value < 0.05. Results Patients with the following SDOH had a statistically significant difference in rates of no-show visits: distance >60min from the HTC (p=0.009), urban vs rural home county (p=0.033), race of patient (p< 0.001), and insurance status (p=0.007). [Figure 1] Further demographic data and analysis included with confidence intervals provided in Fig 1. Conclusions The rate of no-show visits was most affected by patient race, insurance type, distance from HTC, and urban vs rural living conditions. No statistically significant correlations existed within the yearly comprehensive visits, which may be indicative of the shared importance of keeping regularly scheduled appointments between patient and provider when caring for a chronic disease. Interestingly, though previous data in this field has demonstrated rurality as a limitation to care, these findings suggest that an urban setting closer to the HTC presented more of an issue. These findings also help support the benefits of outreach clinics in providing specialized care directly in rural environments, likely reducing no-show rates in this population. This may inspire a similar approach to localized outreach within the urban neighborhoods affected by SDOH limitations to offer clinics where patients are most vulnerable.



