These posters have been presented at meetings in Children's Mercy and around the world. They represent research that was done at the time they were created, and may not represent medical knowledge or practice as it exists at the time viewers access these posters.
-

Concurrent COVID19 pneumonia and systemic inflammatory syndrome in a two-week-old requiring ECMO
Jennie Godwin, Ayan Rajgarhia, Johanna I. Orrick, Jenna Miller, and John M. Daniel IV
Objectives: * Initially, newborns seemed to be relatively spared from severe COVID-19. However, with the emergence of the B.1.617.2 (Delta) variant hospitalization rates among children aged 0-4 years increased by 10-fold by the middle of August 2021. We present a case of a 2-week-old previously healthy preterm, twin, male infant who developed severe COVID-19 pneumonia, subsequent acute respiratory distress syndrome (ARDS), and an inflammatory syndrome requiring VA – ECMO support for 22 days. Methods: * A retrospective chart review was performed after successful weaning from ECMO. Parental permission for a case report was obtained in compliance with institutional standards. Results: * Multiple challenges were encountered during this patient’s 22 days on ECMO. Rising markers of inflammation (LDH, Ferritin, D-dimer, CRP, ESR, troponin) made us concerned for multi-system inflammatory syndrome (MIS) in the setting of pneumonia. This complicated our treatment plan and led to a limited trial of immunomodulating agents in a baby with concurrent viral pneumonia. Dexamethasone, IVIg, and Anakinra were used. After treatment with these agents, clinical improvement began with a slowly clearing chest x-ray (Table 1 and 2) and weaning of ECMO flows. He developed seizures concerning for stroke in the setting of stable markers of coagulation, necessitating faster weaning and earlier ECMO decannulation than desired. Imaging studies showing extensive change to the lung architecture and ultimately required tracheostomy placement. Conclusions: * Severe COVID19 in infants remains a rare condition. Most infants have mild symptoms and recover completely. Unfortunately, some develop severe illness requiring extracorporeal life support. These infants can be successfully managed on ECMO during their acute crisis. The presents of a what appears to be a concurrent hyperinflammatory syndrome presents additional management challenges, but use of immunomodulating agents should be considered in infants.
-
CVST As A Rare Complication of Acute Pediatric COVID-19
Erin Bolen, Jonathan Ermer, and Mukta Sharma
A case report and literature-review derived case series of pediatric central venous sinus thrombosis as a late complication of COVID-19.
-
Improvement in Follow-up Communication for Resident-Identified Patient Safety and Hospital Process Issues
Ross Newman, Angela Etzenhouser, Emily Killough, Danielle Reed, Allison Adam, Michelle Brown, Kelly Meyer, Denise Bratcher, and Nicholas Clark
BACKGROUND: Lean concepts, including Daily Management Systems (DMS), have been adopted by health systems to prioritize high-quality and efficient care. Since 2018, our residency program has utilized a daily readiness huddle (key component of DMS) to prepare inpatient residents for their workday. This is a time when residents can raise administrative and/or clinical patient safety concerns. Concerns unable to be immediately resolved locally are designated as Quick Hits (QH) and escalated through residency and hospital leadership with resolutions cascaded back to frontline providers. With <10% of residents on inpatient services each month, a gap in overall resident awareness of findings from resolved QH exists, posing potential patient safety risks. OBJECTIVE/AIM: We aimed to improve the weekly percentage of findings from resolved QH communicated to every resident (rather than only those in attendance at the daily readiness huddle) from 0% to >95% within 6 months. METHODS: A core team was created consisting of residency program leadership (DIO, Program Directors, Chief Residents). Root causes were identified and guided interventions. Outcome measure was percentage of weekly QH communicated to all residents. Process measure was weekly QH identified for escalation. Findings of resolved QH were shared at bi-weekly residency program meetings/minutes. Plan-Do-Study-Act Cycles included: 1) Standardizing process of identifying QH requiring report-back to all residents, and 2) Audit and feedback to program leadership regarding transmission of resolved QH with adjustment in standard work when needed. Due to rarity of patient safety events, these were unable to be tracked. Run charts assessed improvement over time. RESULTS: Over 20 weeks, 83 QH were identified with 45 requiring escalation beyond residency program leadership for resolution including to physician safety officer and CEO huddles. Outcome measure showed sustained, special-cause improvement from 0% to 100% by Week 15 following Cycle #2 (Fig 1). Process measure remained unchanged at 4.2 QH averaged per week. CONCLUSIONS: Using improvement methodology, we were able to achieve sustained improvement above our goal of communicating findings of resolved QH to all residents. Audit and feedback appeared to have the greatest impact on our outcome measure. Further study is needed, but this closed-loop communication process may also provide beneficial impacts to patient safety.
-
Memory T Cell Populations in Human Leukemia
Sara McElroy, Fang Tao, John Szarejko, and John M. Perry
Background Incorporating the immune system into cancer management is an area of robust research. Treatment modalities aimed at activating cytotoxic T cells against malignancies include immune checkpoint inhibitors, bispecific T-cell engagers, and chimeric antigen receptor (CAR) tumor-specific T cells. Most anti-cancer T cell research is narrowly focused, but knowledge about the nature of diverse sub-populations of T cells in cancer, particularly memory T cells, is vital prior to potential incorporation into therapies. T memory stem cells (Tscm) are of interest due to their longevity and powerful abilities of self-renewal and creating the full spectrum of memory CD8+ T cells, including central memory (Tcm) and effector memory cells (Tem). Objective To determine potential presence and frequency of memory T cell populations in human leukemia at diagnosis and after induction chemotherapy. Design/Method Children’s Mercy Cancer Center Biorepository provided samples from 16 patients with premature B cell acute lymphoblastic leukemia (pre-B ALL) from peripheral blood (PB) and/or bone marrow (BM). Timepoints were diagnosis and day 29 (D29) of induction chemotherapy. Flow cytometric analysis of cytotoxic memory T cell populations was performed and analyzed using descriptive statistics and the t-test. Results Despite sample variability, the absolute cell counts were not significantly different. The live cell percent was lower at diagnosis than D29 (PB- 57.2% vs 79.4%, p=0.001; BM- 41.7% vs 77.0%, p<0.001). T cell frequencies were lower at D29 (PB- 14.8% vs 5.74%, p=0.014; BM- 9.5% vs 5.9%, p=0.217). CD4+ and CD8+ T cells were not significantly different between diagnosis and D29. Among CD8+ T cells, naïve cells markedly increased from diagnosis to D29 (PB- 53.6% vs 82.2%, p < 0.001; BM- 38.8% vs 80.3%, p < 0.001) with a corresponding significant decrease in Tem (PB- 15.1% vs 4.2%, p=0.002; BM- 21.6% vs 4.7%, p < 0.001). Tscm (reported as a % of CD8+ T cells) were detected in all samples at diagnosis (PB range- 0.49-12.2%; BM range- 0.12-4.4%). After induction, two patients had no Tscm detected. The remainder demonstrated varying numbers of Tscm (PB range- 0.038-23.4%; BM range- 0.013-17.4%). Differences between diagnosis and D29 were not significant; however, percentages of Tscm were lower in 9 of 12 patients after chemotherapy. Conclusion Induction chemotherapy led to decreased differentiated CD8+ T cells with recovery of mostly naïve cells by D29. Furthermore, we established the presence of Tscm in most pediatric pre-B ALL samples. The decline of Tscm in most patients requires functional analyses to determine their role in leukemia and potential for use in immunotherapy.
-

Oligodontia, Mandibular Hypoplasia and Microglossia in Pediatric Patients: Review of the Literature and Report of a Case
Gage Williams, Robin Onikul, Jenna Sparks, Neena Patel, Amy Burleson, and Brenda S. Bohaty
Introduction: The combined findings of oligodontia, mandibular hypoplasia and congenital malformation of the tongue (hypoplasia) is relatively rare in children. This presentation discusses the case of a 6-year-old female patient who presented to the dental clinic at The Children’s Mercy Hospital in Kansas City, Missouri for emergent care secondary to gross dental caries. Additional findings at the initial visit were that of oligodontia, microglossia, micrognathia, and mandibular hypoplasia. A review of the medical history indicated that due to the physical anomalies noted at birth, a genetic microarray was completed indicating some variants of unknow clinical significance. As these forms of pathology uncommonly present without a connection to a specific syndrome, further genetic evaluation is warranted. This presentation reviews the clinical findings noted in the case, potential treatment options for future care and the importance of appropriate collaborative care with other medical professionals.
-

Recurrent Primary Spontaneous Pneumothorax Masquerading as a Congenital Pulmonary Airway Malformation in a Young Female
Chandra Swanson, Justin Sobrino, Tolulope A. Oyetunji MD MPH, and Erin Khan
Introduction: Spontaneous pneumothoraxes in children are uncommon, may be idiopathic or associated with underlying pulmonary disease, and can present management challenges. We present a 12-year-old female with recurrent right sided spontaneous pneumothorax in the setting of an asymptomatic SARS-Co-V2 (COVID) infection and imaging concerning for congenital lobar overinflation (CLO) versus congenital pulmonary airway malformation (CPAM), prompting surgical intervention. Case: A 12-year-old pre-menstrual female with remote history of eczema, asthma, and environmental allergies presented from an outside facility with four-days of progressive chest pain and dyspnea on exertion and diagnosis of right-sided spontaneous pneumothorax, improving after pigtail chest tube placement. Physical exam was significant for tall thin body habitus; family history was significant for paternal spontaneous pneumothorax as an adolescent. She was incidentally found to be COVID positive. Chest plain films (CXRs) showed subcutaneous emphysema and persistent right-sided pneumothorax. Clamping trial failed, prompting removal of the pigtail and placement of 12F chest tube with resultant near complete re-expansion. On serial CXRs, a right hilar cystic lucency was newly identified. Chest CT confirmed the right upper lobe (RUL) air-filled cystic structure and abrupt narrowing of the RUL posterior segmental bronchus, concerning for CLO versus CPAM. Chest tube was successfully removed on day 6, and she was discharged home with planned follow-up. Three months later, she was readmitted for recurrent right-sided spontaneous pneumothorax diagnosed after one day of chest pain, cough, and dyspnea. Laboratory testing revealed mild leukopenia and anemia; she was COVID negative. A chest tube was placed and set to wall suction. Due to persistent pneumothorax, this was replaced with a pigtail drain on day 5. CXRs demonstrated persistent cystic RUL lung mass. With her prior COVID infection now resolved, RUL wedge resection was completed via video-assisted thoracoscopic surgery on day 8. She tolerated the procedure well and was discharged on day 10 with resolving pneumothorax. Tissue for pathology results revealed pleural fibrosis and focal hemorrhage without malignancy, most consistent with a ruptured bleb. At one week follow up, she remained stable without complications. Discussion: Pneumothoraxes in tall, thin adolescents are often categorized as primary spontaneous. Most pneumothoraxes resolve with conservative management and often do not require surgical intervention. Congenital lung malformations are a rare secondary cause in children and may be detected on CXR. Chest imaging should be carefully reviewed for congenital malformations requiring specific surgical intervention. These findings, along with the patient’s clinical course, may assist in determining management.
-

Sedation Services Offered at Pediatric Dental Offices in the United States as Reported on Publicly Available Practice Websites
Stefanie Curtis, Jane Witt, Brenda S. Bohaty, Robin Onikul, Amy Burleson, Jenna Sparks, and Neena Patel
Background: As early childhood caries impacts children throughout the United States, restorative dental procedures are often needed. The literature indicates that due to a variety of factors, parents may research their child’s dental condition and try to find options for care that they perceive as least traumatic for their children. These options frequently include sedation and general anesthesia. This background research is typically completed via the internet on public websites. Purpose: The purpose of this investigation was to identify if information regarding specific types of sedation/anesthesia services offered by pediatric dental providers are available on practice websites and to determine if the type of information available differed depending upon practice location. Methods: Pediatric dental practices based in states located in Northeast, Southwest and Western districts as delineated by the AAPD were included in the study. Practices were identified using the ABPD webpage as practices with Board Certified Pediatric dentist practitioners. Specific information regarding the availability of oral conscious sedation, IV sedation, and general anesthesia were assessed and analyzed using descriptive statistics. Results/Conclusions: A total of 432 pediatric dental practice websites were evaluated. 34% of websites analyzed were from the Southwestern district, 30% from the Northeast district and 36% from the Western district. While the majority of all public websites analyzed either did not mention specifically which types of sedation were offered or were unclear about the information, there were however, some statistically significant differences among regions in regard to the type of information available.
-
Treatment of Recurrent Wilms Tumor with Irinotecan/Temozolomide
Meagan Vacek and Terrie Flatt
Background: Despite improvement in relapse free survival (RFS) in recurrent Wilms tumor, the 4-year RFS rate for patients treated with vincristine/dactinomycin/doxorubicin is approximately 40%. Ifosfamide, carboplatin and etoposide are commonly used in relapsed solid tumors, but have significant toxicities and require hospital admission for administration. Our patient focused on quality of life, and this led to exploration of other treatment options. Objective: Describe a case of multiply relapsed Wilms tumor with management on oral irinotecan/temozolomide for improved quality of life and remission for almost 1 year. Design/Method: Case Report Results: The patient is an 11-year-old female diagnosed with Wilms tumor at 6 years of age in Honduras who received approximately 6 months of chemotherapy with Vincristine and a nephrectomy. Staging in Honduras was unknown. Due to financial difficulties, she was unable to continue treatment and family immigrated to the United States. One year after initial diagnosis, imaging revealed large chest mass and intracardiac masses. Biopsy confirmed recurrent Wilms and she received modified NWTS/AREN0534 regimen. Patient responded well to this regimen and then underwent surgical resections and whole lung radiation. At 20 months off therapy, she was found to have a lung nodule, confirmed to be recurrent Wilms tumor. As this was her second recurrence, both patient and family chose a chemotherapy regimen allowing for the best quality of life. She received Irinotecan 90mg/m2/dose PO on days 1-5 and Temozolomide 40mg/m2/dose PO on days 1-5, 8-12, 15-19. She received the 2-drug regimen for 10, 28-day cycles without toxicities or hospitalizations, allowing her to attend school. At the end of cycle 10, she had a third recurrence. Irinotecan is a camptothecin prodrug shown to have activity against adult solid tumors. Topotecan of the same drug class also showed activity in children with favorable histology Wilms tumor with a 48% response rate in heavily pretreated patients. Temozolomide (TMZ) has activity against adult solid tumors with promising results in xenograft models of pediatric solid tumors. O6-methylguanine-DNA methyltransferase (MGMT) is a DNA repair enzyme which inhibits the anti-tumor effect of alkylating agents, like TMZ. Negative MGMT protein expression increases the sensitivity to alkylating agents and can predict the response to temozolomide. Our patient was MGMT negative. Conclusion: Irinotecan/Temozolomide should continue to be explored as an option for relapsed/refractory solid tumors as it can achieve remission for a substantial period while allowing for improved quality of life.
-
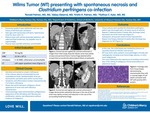
Wilms Tumor (WT) presenting with spontaneous necrosis and Clostridium perfringens co-infection
Ronald Palmen, Abbey Elsbernd, Kristin Palmen, and Kathyrn Kyler
Wilm’s Tumor (WT) is the most common renal malignancy of childhood. The initial presentation of WT may mimic infection or other malignancies with nonspecific symptoms including fever, abdominal/flank pain, or hematuria. We describe a case of WT with spontaneous necrosis obscured by overlying Clostridium perfringens infection. A previously healthy 5-year-old girl presented to the emergency department with a two-day history of flank pain and fevers. She was tachycardic (130 bpm), hypertensive (116/75), and febrile (101.7F). Her abdomen was distended with left-sided flank tenderness without a palpable mass. Initial laboratory testing revealed elevated CRP (70mg/dL) and leukocytosis (22.56 x 109 /L). Urinalysis showed 5-10 WBCs but was otherwise normal. A CT abdomen/pelvis with contrast demonstrated a mass-like structure in the left upper quadrant, surrounding and splaying the left adrenal gland with inferior displacement of the left kidney. The patient was hospitalized for evaluation and received empiric ceftriaxone. Additional laboratory studies were obtained including urine cultures, plasma normetanephrine and metanephrine levels, as well as Vanillylmandelic Acid (VMA) and Homovanillic acid (HVA) levels. All were within normal limits. Her symptoms, leukocytosis and CRP improved with resolution of fevers after 5 days. Given the ambiguous clinical picture favoring infectious versus oncologic diagnoses, open surgical biopsy of the left kidney and surrounding mass was performed. Pathology demonstrated a phlegmonous appearance of the left kidney and fibrovascular proliferation with inflammation and no evidence of malignancy. Tissue cultures were positive for Clostridium perfringens. At discharge, the patient transitioned to a 10-week course of cefixime for C. perfringens kidney infection with outpatient follow-up. Repeat CT abdomen/pelvis obtained 4 weeks after discharge demonstrated decreased size of the renal mass. In outpatient follow-up, repeat ultrasounds minimally improved, therefore a second renal biopsy was obtained 13 weeks after discharge. The biopsy identified monomorphic small cells in varying stages of cell death with positive WT1 protein, consistent with WT. This case features an unusual presentation of WT with spontaneous necrosis and concomitant C. perfringens infection. Our patient’s presentation was suspicious, however her initial negative biopsy was masked by the presence of secondary bacterial infection and necrosis, leading to delayed oncology referral and treatment. This case underscores the importance of avoiding confirmation bias in the setting of ambiguous clinical presentations. WT may mimic other pediatric renal pathologies clinically and radiologically, such as renal hemorrhage, abscess, or other malignancies. This poses a diagnostic challenge for providers, particularly when both infection and malignancy are observed.
-

17-year-old ballet dancer with 4 years of right upper extremity pain
Mariah Sisson and Brian S. Harvey
History:No known injury. Intermittent, dull, radiating. Starting at the shoulder and moving to the medial elbow, but sometimes only at the medial elbow with numbness of the 4th/5th digits. No limitations in ballet. Extended course to see Sports Medicine. PCP - failed treatment for herpetic whitlow, referred to dermatology. Dermatology - bilateral Raynaud's syndrome & Pernio, referred to rheumatology. Rheumatology - having RUE numbness, referred to neurology & PT. Neurology - tenderness to palpation at the anterior shoulder, referred to Sports Medicine. PT - getting stronger, but symptomatically making minimal improvement. PE:Cardiac: capillary refill normal. MSK: RUE: Inspection: No erythema, edema, or bruising. Lower trapezius wasting visible when examining back/scapula. Palpation: Tenderness at medial epicondyle but not same pain she has previously experienced. No tenderness to palpation throughout remainder of RUE. ROM: Full ROM without pain or numbness. Strength: Normal strength. Special Tests: Spurling's negative, Roos negative, Adson's positive with loss of palpable radial pulse. Differential:Thoracic Outlet Syndrome, Cervical Neuropathy, Right Shoulder Tendinopathy, Scapular Dyskinesia, Medial Epicondylitis. Discussion:Initial presentation was interesting with overall non-specific symptoms and many specialists who had new findings, including bilateral Raynaud's syndrome. Patient was unable to truly localize if the pain was from her neck, shoulder, or elbow, but endorsed pain at times in all these locations and had no symptoms on day of clinic visit. It wasn't until the positive Adson's test that the diagnosis started to become clearer, or at least moved thoracic outlet syndrome to the top of the differential diagnosis. Concern for thoracic outlet syndrome guided further management.
-

A rare cause of elbow pain with a controversial name
Thomas Munro and Brian Harvey
History: 13-year-old right hand dominant male presenting with 1-year concerns of bilateral elbow locking, popping, and pain. Right elbow tends to be affected more frequently than left. Patient states that at random, when he is trying to extend at the elbow joint, his elbows will "lock up". He will not be able to extend past this region and has significant pain when this occurs. He has to proceed back into elbow flexion and again try to "push through" into full extension. This will result in a loud pop followed by about 5-10 minutes of pain which slowly resolves. This happens typically once a day for about 4 days out of the week. He denies any mechanism of injury and specifically denies any previous elbow contact injuries. He is in 8th grade and participates in baseball, basketball, and tennis. Physical Examination: Constitutional- Well-developed well-nourished. MSK: Bilateral Elbow. Neuro- sensation intact in the distal UE bilat Vascular- 2+ pulses in upper/lower extremity. Inspection - no swelling, bruising, erythema or skin changes. Palpation: -Non-tender: medial/lateral epicondyle, radial head, olecranon, triceps. - Tender: Radio-capitellar Joint, Flexor-Pronator Complex, Extension-Supination Complex. Range of motion of the elbow -Normal: flexion, extension, pronation, supination. Strength- normal elbow flexion, elbow extension, wrist flexion, wrist extension, pronation/supination. Special Testing Test: Valgus- no pain, Varus- No pain, Moving Valgus- no pain, Tinel's test negative Differential Diagnosis: 1. Capitellar OCD 2. Panner disease 3. Loose bony fragment in the joint space 4. Repetitive elbow subluxation 5. Arteriovenous malformation Tests & Results: After obtaining history and completing the physical exam bilateral elbow x-rays were ordered. X-ray read from radiology showed No fracture or dislocation involving the bilateral elbows with clinical overread and physical exam correlation showing concerns for possible trochlear OCD lesions bilaterally. MRI was obtained showing mild so called fishtail deformities of the bilateral humeri. Final/Working Diagnosis: Hegemann's Disease (post-traumatic disturbance of the epiphysis of the humeral trochlea). Discussion: Hegemann's Disease is a rare diagnosis. It presents with elbow pain, locking sensation, decreased range of motion, and sometimes swelling. A discussion has begun on whether this diagnosis would more properly exists on the same playing field as the rare but more well-known, fishtail deformity. The etiology of both have been postulated to be secondary to disruption of the vulnerable vascular supply of the trochlea. It has been proposed that these two diagnoses be lumped together and more accurately termed post-traumatic disturbance of the epiphysis of the trochlea. Our patient providers another example of such a deformity without a clear inciting injury. It is unique in its bilateral nature. Outcome: This patient was instructed on activity modification (held from sport and instructed to avoid throwing and arm weight-bearing activities) and began formal PT. The rarity of this disease lends to the lack of a consensus treatment though some form of activity modification seems to be common. Return to Activity and Follow-Up: Patient has yet to return to full activity and is continuing physical therapy. In our patient it is possible that if vascular supply recovers before closure of the physeal plate, the injury will remodel into a normal trochlea but could also still ultimately develop a fishtail deformity.
-

Caregiver Mental Health Screening in a Pediatric Feeding Clinic
Dana Bakula, Laura Slosky, Kelsey Dean, Ann M. Davis, and Sarah T. Edwards
Introduction: One in four adults have mental health (MH) problems. Caregivers of children with feeding problems are at even higher risk for mental health (MH) problems, including depression, anxiety, and posttraumatic stress. Caregiver MH concerns have a negative impact on caregiver and child quality of life and are specifically linked to suboptimal child feeding practices. Thus, it is critical to identify caregiver MH problems in pediatric feeding settings. However, it can be challenging to comprehensively screen for caregiver MH in a busy pediatric feeding clinic. This emphasizes the importance of a feasible and brief method for screening caregiver MH. Methods: From 2019-present our multidisciplinary feeding clinic has been administering a 2-item caregiver MH questionnaire to caregivers presenting for a new visit with their child. The questionnaire asks if one or more of the primary caregivers in the home has a MH problem, and what the problem is. We descriptively evaluated these screenings compared to base rates in the literature. Results: Caregivers of 327 children were screened, and 40% of caregivers endorsed at least one caregiver in the home had a mental health problem, such as depression, anxiety, or PTSD. Among caregivers of children under the age of one year, 45% of caregivers reported MH problems (many of which were post-partum depression and anxiety). These data are in line with rates observed in the literature, indicating that roughly 40% of caregivers of children with feeding problems have MH problems. Conclusions: This two-item screener shows promise in identifying caregiver MH problems, as positive screens were similar to observed rates in the literature. However, additional research is needed to evaluate sensitivity and specificity of this measure. Although not a perfect screener, this two-item screener was quite feasible to implement, as it easily integrated into new visit paperwork. Caregivers who screen positive meet our team social worker and/or psychologist to discuss their MH concerns and connect caregivers with resources. More research is needed to refine best practices in caregiver MH screening in pediatric feeding settings. Further, given these high rates of MH problems, point of care interventions to address caregiver MH in clinic would be ideal, and would reduce barriers to seeking care in the community. This may be particularly important for caregivers of infants, given high rates of postpartum MH problems.
-

Healthcare Needs and Experiences of Detained Youth
April McNeill-Johnson, Zuri Hudson, Brittany Moore, Dumebi Okocha, Megha Ramaswamy, and Kimberly A Randell
COVID-19 : Perspectives from Youth in Detention Background: The COVID-19 pandemic amplified health disparities among youth in detention. Understanding perspectives of these youth on the pandemic and COVID-19 vaccination may identify strategies to mitigate pandemic-related health disparities in this group. Objective: To explore perspectives on the COVID-19 pandemic, effect on detention experience & the COVID vaccine among youth in detention. Methods: This is a secondary analysis of a study examining healthcare needs and experiences of youth in detention. We recruited a convenience sample of youth (14-17 years) detained in urban midwestern juvenile detention centers from January-November 2021. We conducted semi-structured individual interviews & used a thematic analysis approach to code interview transcripts, after which codes were consolidated into themes. In early interviews, participants spontaneously discussed the COVID-19 pandemic, prompting addition of interview questions to further explore this. Participants completed an anonymous demographic questionnaire at the conclusion of the interview. Results: 15 youth (Table 1) discussed COVID-19 to date, with interviews ongoing. Youth had varied opinions on the gravity of the pandemic. Most thought that COVID-19 was a significant issue, but some felt the pandemic was fictitious. Youth obtained information primarily from family, friends, social media, and commercial news sources. Most youth voiced that they would not get the COVID-19 vaccine. Many expressed general distrust of the vaccine. Concerns included the speed of vaccine development and implementation and misconceptions about how the vaccine works. Some also felt they are immune to COVID-19 due to their youth and health. Among those who were vaccinated, parental preference and personal gain (i.e., travel, sport participation) drove vaccination acceptance. Youth suggested targeted educational strategies to increase youth vaccine uptake. Youth described negative impacts of the pandemic on their detention experiences. Visitation was limited with bans on personal touch, halts placed on packages being delivered from the outside community, and a 10-day quarantine was mandated at detention entry. See Table 2 for illustrative quotes. Conclusions: Youth in detention have varied perspectives on the gravity of the COVID-19 pandemic. Vaccine misconceptions and perceived lack of vulnerability to COVID-19 contributed to vaccine hesitancy. Vaccine uptake by youth in detention may be improved by partnering with parents, highlighting personal gain, and youth-targeted education.
-

Identifying Predictive Factors for Patients Transferred From Floor to PICU within 24 hours of Admission by a Pediatric Critical Care Transport Team
Gina Patel, Lisa Carney, Brian S. Olsen, and Jennifer Flint
Abstract Objectives: Appropriate triage and disposition during transport can reduce the need for unplanned transfers to the pediatric intensive care unit (PICU) within 24 hours of admission. The pediatric early warning score (PEWS) is utilized to monitor for inpatient clinical deterioration and acuity during transport at our hospital. We sought to determine predictive factors of patients admitted to the inpatient ward who required PICU transfer within 24 hours following transport by Children’s Mercy Critical Care Transport (CMCCT) team. We hypothesized patients with respiratory illness and PEWS > 4 during interfacility transport are at higher risk of PICU transfer within 24 hours of admission. Methods: A retrospective, case-controlled chart review of 100 total transports by CMCCT between January 2018 - December 2020 was performed. We included patients 1 month to 18 years of age admitted to the inpatient ward with respiratory illness and excluded patients with congenital heart disease. PICU transfers within 24 hours were compared to the control group who did not require PICU transfer. Metrics from pre-transport, transport, floor and first 24 hours after PICU transfer were recorded into the Research Electronic Data Capture Database (REDCap). Results: PICU transfers had a median PEWS score of 4 [3,5, p= 0.036] compared to a PEWS of 3 [2,4, p= 0.036] in patients who remained on the floor. PEWS scores were grouped into green (0-2), yellow (3) and red zone ( > 4) based on our institutional floor protocol for multivariate analysis. A trend towards higher transport PEWS scores for PICU transfers within 24 hours was noted with 30/50 (OR 2.02, p= 0.141) having the highest transport PEWS in the red zone as compared to the control group but was not statistically significant. A trend towards higher admission PEWS for PICU transfers was also noted. A higher floor admission PEWS in the red zone was statistically significant for PICU transfer with 23/50 (OR 4.95, p= 0.001). There were no differences between the 2 groups related to prematurity (p= 0.795), home oxygen (p= 0.999), high flow nasal cannula (p= 0.262), or continuous beta agonist (p= 0.454). Patients transferred to the PICU did have lower weights (11.7, [7.8, 17.7], p= 0.09) compared to those who remained on the floor (median 14.7, [IQR 10.3,20.1], p = 0.09), however, this was not statistically significant. Conclusion: Our analysis showed a trend towards higher transport PEWS for patients who required subsequent PICU transfer but was not statistically significant, suggesting PEWS alone may not be a useful scoring tool to determine patient disposition during transport. A higher PEWS score after hospital admission on the general pediatric floor was associated with PICU transfer. Future directions should include additional study with larger sample sizes analyzing other risk factors or interventions during interfacility transport that might predict PICU transfer after admission to the floor.
-
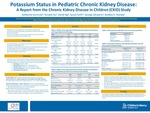
Potassium Status in Pediatric Chronic Kidney Disease: A Preliminary Report from the Chronic Kidney Disease in Children (CKiD) Study
Katherine L. Kurzinski, Yunwen Xu, Derek NG, Susan Furth, George Schwartz, and Bradley A. Warady
-

Rare variants in renal developmental genes and the risk of hypertension and CKD: a UK Biobank study
Benjamin Spector, Byunggil Yoo, Neil Miller, and Laurel K. Willig
Background: Prior studies show chronic kidney disease (CKD) is heritable but only a few common variants have been associated with CKD and kidney dysfunction. Much of CKD heritability remains unknown and limited studies have explored the role of rare genetic variants in this missing heritability. Objectives: Identify rare genetic variants in renal developmental genes associated with hypertension and CKD. Methods: We examined the association between rare variants in 58 candidate genes from five renal developmental compartments and presence of CKD and elevated blood pressure (BP) in 49,989 individuals using whole exome sequencing and phenotypic data from the UK Biobank. Criteria for qualifying rare variants included a minor allele frequency < 0.1% and classification as pathogenic, likely pathogenic, or variant of uncertain significance (VUS) using in-house characterization software. Logistic regression models were generated for each compartment to determine the predictive ability of qualifying variants for the outcomes of elevated BP and CKD, with additional subgroup analysis by genetic ethnicity. Genes were selected for inclusion in regression models based on p < 0.25 using Chi-square univariate analysis. Genes included for each developmental compartment’s regression model are summarized in Tables 1 & 2. Results: Qualifying variants in 5 genes across 3 developmental compartments were significant predictors of elevated BP; qualifying variants in 4 genes across 4 developmental compartments were predictive of CKD. In subgroup analysis of individuals genetically identified as Caucasian, qualifying variants in 4 genes across 3 compartments were predictive of elevated BP; qualifying variants in 3 genes across 2 compartments were predictive of CKD. For individuals genetically identified as non-Caucasian qualifying variants in 3 genes across 2 compartments were predictive of elevated BP; qualifying variants in 6 genes across 2 compartments were predictive of CKD (Tables 1 & 2). The distribution of qualifying variant types (i.e. pathogenic, likely pathogenic, VUS) within genes containing rare variants predictive of disease were predominately VUSs (Figure 1). Conclusion: Rare variants in some renal developmental genes are associated with elevated BP and CKD and may help explain a portion of the missing heritability. However, the significances of variants differ by ethnicity, and the majority are classified as VUSs requiring further characterization.
-

Rates of Physical Abuse Screening and Detection in Infants with Brief Resolved Unexplained Events (BRUEs)
Angela Doswell, James Anderst, Joel Tieder, and Henry T. Puls
Background: “Apparent Life-Threatening Events” (ALTEs) have been associated with child physical abuse (CPA). In 2016, “Brief Resolved Unexplained Event” (BRUE) and the development of its clinical guidelines and risk-stratification replaced ALTE. However, it is unknown if there is a similar association between BRUEs and CPA. Objectives: To determine the rate of CPA in infants presenting with a BRUE, examine differences between infants with and without CPA, and to examine rates of diagnostic testing used to detect CPA. Methods: This study was part of the BRUE Research and Quality Improvement Network, which is composed of 15 academic and community hospitals. Subjects were infants presenting with BRUE in emergency department or inpatient settings and followed from BRUE presentation through the first year of life. The primary outcome was CPA diagnosis at either initial BRUE or subsequent presentations. The secondary outcomes were minor evidence of trauma and diagnostic testing used to detect CPA (head imaging, skeletal survey, and/or liver transaminases) at initial BRUE presentation. Chi-square tests assessed for differences. Results: Of the 2036 infants presenting with a BRUE, 7 (0.3%) were diagnosed with CPA. Only 1 (<0.1%) infant was diagnosed with CPA at initial BRUE presentation. Infants diagnosed with CPA were more likely to exhibit color change (100% vs. 51.1%, p=0.01) and have minor evidence of trauma (14.3% vs. 0.3%, p<0.001) at initial BRUE presentation. There was no difference in CPA diagnosis by BRUE risk stratification. There were 7 (0.3%) infants with minor evidence of trauma, only 1 of whom was diagnosed with CPA. Of all infants, only 6.2% underwent head imaging, 7% skeletal survey, and 12.1% liver transaminases. Skeletal survey was more likely to be performed if there was minor evidence of trauma (42.9 vs. 6.9%, P <0.001) or a concerning social history (13.9% vs. 5.9%, p <0.05). Head imaging was more often performed if infants had minor evidence of trauma (71.4% vs. 6.0%; p< 0.001), family history of sudden unexplained death (10.2% vs. 6.3%; p= 0.047) or concerning social history (22.8% vs. 5.4%; p< 0.001). Conclusion: There was a lower rate of CPA in infants at initial BRUE presentation (<0.1%) than in infants with ALTE, although testing rates at initial BRUE presentation were also low. Minor evidence of trauma and concerning social history appeared to raise suspicion for and initiate diagnostic testing to detect CPA. Further research is warranted to systematically identify infants with BRUE at increased risk for CPA.
-

Self-Reported Sexual Behavior in A Pediatric Gender Clinic Sample
Mirae J. Fornander, Anna Egan, and Christine Moser
Introduction Previous studies of transgender/gender diverse (TGD) youth indicate differences in rates of sexual behaviors between TGD youth and their cisgender peers. However, few studies have reported the sexual behavior and preferences of TGD youth in a large clinic sample, and no studies, to our knowledge, have utilized questionnaires that do not assume the sex or gender of one’s sexual partner. The current study aims to explore the self-reported sexual behavior of TGD youth presenting for gender-affirming medical care. Methods Retrospective chart review of 589 patients (ages 12-22, M= 15.92, SD= 1.54; 72.9% assigned female sex at birth (SAB)) presenting for an initial visit at a pediatric transgender clinic from 2015-2021. Patients self-reported their gender identity, sexual behavior, sexual partners, and sexual interests via a REDCap electronic survey. Results Rates of dating (39.3% v 68.3%; X2=216.06, p< 0.0001) and sexual intercourse (22.9% vs 39.5% X2=65.69, p< 0.0001) among TGD youth were significantly lower than national norms (Kann et al., 2018). Rates of self-reported being forced to have sex among TGD youth was 7.6% and did not differ significantly from national norms (6.9%, ns; Kann et al., 2018). In the last year, TGD youth reported having one sexual partner (58.2%), 2-3 partners (19.4%), no partners (11.2%), 4-7 partners (8.2%), 8-10 partners (2.2%), and more than 10 partners (0.7%). Most TGD reported they were not likely to have sex in the next year (60.2%). TGD youth reporting using their mouth (11.2%), vagina (7.1%), penis (2.5%), anus (2.2%), or none of these body parts (0.7%) during sex. The gender of TGD youth partners included cisgender female (6.6%), cisgender male (5.8%), gender nonconforming female SAB (2.2%), transgender male (2.0%), gender nonconforming male SAB (1.4%), and transgender female (0.8%). Conclusions Results suggest that rates of dating and sexual intercourse among TGD youth are significantly lower than national norms. Clinically, results support screening for sexual behaviors and health among TGD youth and utilizing measures that do not assume the sex or gender of one’s partners. Future research should aim to develop a standardized measure of sexual behavior that addresses the unique needs of TGD youth to improve the accuracy of reporting in this population.
-

Trends in Proportions of Female Representation at American Society of Pediatric Nephrology Pediatric Academic Society Meetings 2012-2021
Bahar Barani Najafabadi, Dave Selewski, Danielle Soranno, and Darcy Weidemann
-

Ultrasound Guided Peripheral IV Access Curriculum for the Pediatric Emergency Department: A Pilot Study.
Samuel Dillman, Frances Turcotte Benedict, and Christopher S. Kennedy
Ultrasound Guided Peripheral IV Access Curriculum for the Pediatric Emergency Department: a pilot study. Background: Up to 50% of children have difficult venous access. Studies in the Pediatric Emergency department (PED) have shown that ultrasound guided peripheral IV (USGPIV) access has decreased IV access time and ED length of stay. Barriers for use include lack of training and comfort with the procedure. Objectives/Goal: Our objectives are to pilot and evaluate USGPIV training for Pediatric Emergency Medicine (PEM) physicians and nurses. Methods/Design: The course included a 4-hour, hands-on session with US IV training using a blue phantom task trainer in conjunction with the Vascular Access Team (VAT) for PEM physicians and nurses. Participants’ skills were accessed by the trainers in two ways: 1. Consensus-based stepwise checklist (345-460 Excellent, 230-344 Good, 229-116 Fair, 0-115 Poor) 2. Global assessment of performance (1=Novice to 5= Expert). Obtained pre and post course and participant self-assessments by web-based survey (RedCap). Self-reported confidence with USGPIV was collected pre and post training and 3 months after training. Pre-post confidence mean scores were calculated for each participant and compared using a paired t-test (p value of <.05). Data collection included discipline and prior traditional IV or ultrasound experience. Course-based questions included if the training was an appropriate use of time, would be recommended to colleagues, and if it would be utilized in future practice. (5-point Likert scales: e.g. Novice to expert). Results: 23 providers were trained, 65% PEM physicians and 35% nurses. Skills assessment results for all participants scored an excellent rating (mean of 439) with subjective ratings most frequently indicating a competent trainee. There was a statistically significant increase in self-reported confidence in USGPIV placement post training (p < 0.0003). Three months post survey, confidence in skills significantly decreased. Learners recommend training to other providers, thought it was a good use of their time, and agreed they would utilize USGPIV access in their clinical practice. Conclusions: The training to date has shown acceptability, perceived increase in confidence, and excellent scores on training evaluations. Confidence decreased 4 months post training. Further steps include quality improvement of decreasing time to IV access in difficult access patients through utilization of USGPIV with patient data showing a 56-minute time to IV access for difficult venous access patients at our institution.
-

Evaluation Of The Outcomes Of Oral Challenges To Azithromycin, Cephalexin And Trimethoprim-Sulfamethoxazole In Pediatrics
Hannah N. Neuhaus, Jordan Heath MD, and Salman Aljubran
Rationale: Antibiotic hypersensitivity complicates treatment for various infections and leads to long-term healthcare costs and antibiotic resistance. Data regarding the outcomes of oral challenges to trimethoprim-sulfamethoxazole, azithromycin and cephalexin are limited in Pediatrics. The goal of this study was to characterize the outcomes and safety of oral challenges to these antibiotics in Pediatrics.
Methods: A retrospective chart review was performed of pediatric patients who underwent oral challenges to cephalexin, azithromycin and trimethoprim-sulfamethoxazole in Allergy Clinic over the last 12 years.
Results: Ten patients underwent oral challenge to trimethoprim-sulfamethoxazole and all were successful. Thirteen patients underwent oral challenge to azithromycin and twelve were successful. One patient failed the oral challenge with development of urticaria within 5 minutes on first dose. Twelve patients underwent oral challenge to cephalexin. Ten patients successfully passed the oral challenge while two failed. Of the two who failed, one patient later developed signs of viral illness and the second developed pruritic rash shortly after first dose and was transitioned to a desensitization protocol.
Conclusions: Hypersensitivity to trimethoprim-sulfamethoxazole, azithromycin and cephalexin have significant impact on treatment for infections and require evaluation and de-labeling if possible. Overall, this study demonstrated that oral challenge to azithromycin, cephalexin and trimethoprim-sulfamethoxazole is a safe procedure to perform in select pediatric patients and can be done safely in the outpatient setting.
-

Extubated VV-ECMO for COVID-19 ARDS in an Immunosuppressed Pediatric Renal Transplant Patient.
Johanna I. Orrick, Cara Holton, Tara Benton, and Jenna Miller
Extracorporeal membrane oxygenation (ECMO) for coronavirus disease 2019 (COVID-19) associated acute respiratory distress syndrome (ARDS) in adults is common, and outcomes are similar to those for non-COVID-19 ARDS on ECMO1. However, children are much less likely to have severe COVID-19 disease, and thus the need for extracorporeal support is rare2,3. Even pediatric solid organ transplant recipients with active COVID-19 infections typically do not require ECMO.4 We present the case of an immunosuppressed pediatric patient with COVID-19-related ARDS who had an excellent outcome on VV-ECMO. An 11-year-old female with a history of polycystic kidney disease status post renal transplant three years earlier was admitted to the pediatric intensive care unit (PICU) with COVID-19 pneumonia. She developed severe ARDS and required intubation on hospital day (HD) 19. The patient's condition deteriorated despite trials of prone positioning, nitric oxide, and neuromuscular blockade. Due to her refractory hypoxemia, she was cannulated to venovenous (VV) ECMO on HD 28 utilizing a 27 french Avalon bi-caval dual lumen cannula. Laboratory testing demonstrated severely impaired immune function due to her baseline immunosuppressive regimen of mycophenolate, prednisone, and tacrolimus. In addition, she had received B cell depleting therapy with Rituximab several months prior to admission for management of transplant rejection. During her ECMO run, she developed pulmonary aspergillus in addition to her COVID-19 infection. Thus, the overall treatment goal was to minimize immunosuppression sufficiently to manage COVID-19 and aspergillus infections while not triggering rejection of her transplanted kidney. On admission, her mycophenolate dose and tacrolimus trough goal were reduced. When her status worsened shortly after intubation, mycophenolate was discontinued, and tacrolimus trough goal was further decreased. For treatment of acute COVID-19 pneumonia she received remdesivir, dexamethasone, tocilizumab, and convalescent plasma. Farther into her course, she was also treated for suspected MIS-C with anakinra, IVIG, and methylprednisolone. COVID-19 polymerase chain reaction (PCR) and cycle threshold times were monitored weekly. Gradually her cycle threshold times increased, and her COVID-19 PCR became negative on HD 61. With this laboratory and clinical improvement, her mycophenolate was restarted at 50% of the previous dose, and the tacrolimus trough goal was increased to its previous level. There were no concerns for graft rejection during her hospitalization. However, continuous renal replacement therapy (CRRT) was required in tandem for the first four days of extracorporeal support. Following this, she maintained good renal function with her transplanted kidney for the remainder of her hospital course. Five days after VV-ECMO cannulation, she was extubated to a high-flow nasal cannula. With weaning of neurosedative infusions, she was able to participate in pulmonary clearance and physical rehabilitation while on ECMO. With aggressive rehab she could sit on the edge of her bed and even transfer to a chair with assistance. After 33 days of ECMO support, she was decannulated on high-flow nasal cannula. She left the PICU on HD 83 and was discharged home without supplemental oxygen on HD 104. Our case experience suggests that extubated VV-ECMO can be a safe and effective rescue therapy for COVID-19-related ARDS in children, even in the setting of immunosuppression. Modification of immunosuppressive regimens in the setting of acute COVID-19 disease is not well described in the pediatric population.3 Our case study demonstrates it is possible to balance the risk of transplant rejection with infection control and ECMO therapy. Immunocompromised pediatric patients with COVID-19 can be considered candidates for ECMO support.
-
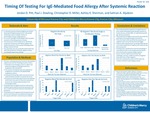
Timing Of Testing For IgE-Mediated Food Allergy After Systemic Reaction
Jordan Pitt, Paul J. Dowling, Christopher Miller, Ashley Sherman, and Salman Aljubran
Rationale: A refractory period of falsely negative testing can occur following a systemic allergic reaction to Hymenoptera sting. As a result, blood specific IgE and/or skin prick tests (SPT) for other allergens are often delayed. This retrospective chart review aims to identify the proportion of patients with falsely negative test results in the 6 weeks following an allergic reaction to food, and factors that may affect it. Methods: One hundred fourteen pediatric subjects met inclusion criteria. Each had a convincing history of food allergy with a systemic allergic reaction and was tested to the culprit food within 6 weeks. The proportion of negative tests for each testing modality was compared. Subjects testing negative were also compared to those testing positive. Chi-square and Fisher’s exact tests identified differences between groups. Results: Seventeen of 79 blood IgE tests (21.5%) and 6 of 35 SPT (17.1%) were negative, with no significant difference between the two tests (p-value 0.591). The distribution of trigger foods was significantly different in subjects with negative versus positive tests. Importantly, there were no subjects who tested falsely negative to tree nuts out of the 38 blood IgE tests and 13 SPT for tree nut allergy. Conclusions: The proportion of falsely negative tests in the 6 weeks following systemic allergic reactions to food is similarly low in both testing modalities. This proportion was even lower in subjects with tree nut allergy. Thus, testing can be considered to confirm food allergy in most patients with a convincing history during the weeks following a systemic reaction.
-

Getting Back to Global Health; Lake Atitlan, Guatemla
Kyra L. McCarty
Describes pediatric resident's exposure to the Guatemala health service and medical education system.
-

Elevated stool inflammatory markers in early onset polymorphic post-transplant lymphoproliferative disease following orthotopic heart transplant
Jeremy Stewart, Keith August, and Thomas M. Attard
Acute gastrointestinal hemorrhage in the context of a recent organ transplant with immunosuppression, antibiotic exposure, drug exposures and other comorbidities is a challenging clinical scenario with coordinated multidisciplinary effort needed to optimize management and outcomes. We present a patient with recent solid organ transplant with severe acute gastrointestinal bleeding attributable to EBV associated post-transplant lymphoproliferative disease. The patient is a 13-year-old Female with Williams syndrome who is EBV negative and CMV positive who received an EBV/CMV positive orthotopic heart transplant 5.5 months prior to presentation. She presented with bloody diarrhea, anemia (7.8 gm/dL), hypovolemia, and acute kidney injury (BUN 25 mg/dL - baseline 8-12) and admitted for IV fluid replacement, blood transfusion, and IV Iron infusion. Fecal calprotectin was 938 mcg/g and stool lactoferrin was 379.8 mcg/mL. MR enterography demonstrated inflammatory changes of the terminal ileum without evidence of stricture and prominent (reactive) mesenteric lymph nodes. EGD and Colonoscopy on day 8 of admission revealed multiple, sessile, semi-pedunculated, moderately vascular and raised lesions with central umbilication and granulation tissue at the apex ranging in size from 0.3 to 1 cm in the stomach, duodenum, terminal ileum, and the colon with similar findings in the small bowel on capsule endoscopy. She also had esophagitis, non-specific mild, chronic gastritis, normal terminal ileal and colonic mucosal biopsies with no inflammatory changes. Margin biopsies were infiltrated with a variable lymphoid cell population throughout the lamina propria, glandular architectural distortion, and focal gland destruction. The lymphoid cells were variable in size with small (CD3/CD43 positive) and large (CD20/CD43 positive) lymphocytes with vesicular chromatin and occasional prominent nuclei. EBER CISH was positive in many of the abnormal cells. She was diagnosed with EBV positive, polymorphic post-transplant lymphoproliferative disease (PTLD). Following a pre-treatment PET/CT scan revealing abnormal activity throughout the neck, chest, abdomen, and pelvis, she was started on rituximab, maintained tacrolimus with a goal serum level of 5-10, whereas MMF was withheld. PTLD is caused by proliferation of lymphoid or plasma cells and is the most common malignancy in the pediatric transplant population. The hallmark is EBV infection in the context of immunosuppression, occurs in approximately 2-15% of organ transplant recipients, can present with fever, lethargy, weight loss, generalized malaise, and lymphadenopathy but may also present with symptoms specific to the organ affected. Outside the gastrointestinal tract, PTLD can develop in the lymph system, central nervous system, lung, and liver. Gastrointestinal involvement includes bleeding, anemia, hypoalbuminemia, protein-losing enteropathy, and diarrhea. Treatment includes reduction in immunosuppression followed by a chemotherapeutic agent such as rituximab. Treatment can also involve surgical resection, radiation, anti-CD20 antibody therapy, or cytotoxic T-cell therapy. Outcomes vary by transplanted organ and can result in organ failure secondary to rejection and even death but with higher overall survival rates in children. The case presented is interesting insofar as the early presentation is atypical and it also illustrates the elevation in stool inflammatory markers, both lactoferrin and calprotectin, which has not previously been reported in the literature. The elevated stool markers are also interesting given the lack of gross morphologic or biopsy proven inflammation in non-lesion pathology. Our report underscores the utility of stool inflammatory markers in gastrointestinal bleeding in the solid-organ transplant recipient.



