These posters have been presented at meetings in Children's Mercy and around the world. They represent research that was done at the time they were created, and may not represent medical knowledge or practice as it exists at the time viewers access these posters.
-

Grading of Improvement in Hypsarrhythmia with Standard Epileptic Spasms Treatment at a Large Pediatric Tertiary Care Center
Julie Grace Gianakon, Roha Khalid, and Mohammed Ilyas
Background Epileptic spasm is a peculiar type of epileptic seizure, entailing the clinical spasms and a characteristic electroencephalogram (EEG) abnormality often called hypsarrhythmia or its variants. The main goal of epileptic spasm treatment with standard therapy is to suppress clinical spasms and abolish the hypsarrhythmia and its variant EEG pattern. This interictal EEG pattern frequently heralds developmental regression. The elimination of hypsarrhythmia is a principal goal of therapy and a key outcome measure in clinical trials. There have been several studies in the interpretation or grading of hypsarrhythmia (Watanabe et al.1993 & Jeavons & Bower et al.1961). Still, there have been no studies in the grading of electrographic improvement with the standard treatment and its effects on the outcome, mainly in terms of remission vs. relapse. Objective: We aim to assess the electrographic improvement of hypsarrhythmia and its variants with standard hormonal (ACTH or prednisone) and Vigabatrin therapy based on the standard EEG scoring system (Kramer et al.1998). It is also generally accepted that outcome depends upon the underlying disease, so we selected patients with common etiologies (Cryptogenic, Down Syndrome, and Tuberous Sclerosis) and determined the EEG features predicting remission or relapse of epileptic spasms.
Methods: This is a retrospective chart review examining several EEGs before and after treatment using a standard scoring system (Kramer et al.1998) for a follow-up period of at least 6months to 1year. We analyzed different EEGs and graded them based on a standard scoring system on pretreatment EEG (at the time of diagnosis) and post-treatment EEG changes (1-2wks, 2-3 months, or 6-12 months) in patients with epileptic spasms who received standard treatment.
Results: Of 24 patients with epileptic spasms, 18 had EEG improvement of over 75% with resolution of spasms. Four had less than 50% improvement with refractory or recurrent spasms. Two patients had improvement between 50 and 75%. One had resolution of spasms, while the other had recurrent spasms.
Conclusions: Patients with sustained improvement in EEG over at least 3-6 months of about > 75% were associated with spasms remission. Patients in whom the improvements were less than 50% continued to have ongoing spasms. These results highlight the need for the level of aggressiveness and close follow-up depending on the degree of EEG improvements with standard therapy.
-

Standardizing Resident Education on GI service
Jennifer Halma and Kenneth Schmidt
Introduction: The pediatric residency curriculum at Children’s Mercy Hospital is standardized to offer each trainee the same rotational experience. As a result, each resident spends one month on the inpatient gastroenterology (GI) service during training. This invites variability in the quantity and quality of GI education that residents receive. Therefore, there is a need to design a standard curriculum to provide comprehensive GI education. The aim of this project is to standardize resident education by identifying most requested topics and providing didactic education to increase resident general GI knowledge. Methods: Each month, residents were provided with a survey to assess comfort level in taking care of GI patients and writing total parenteral nutrition (TPN) orders, along with requesting their most desired didactic topics. These topics were then prioritized to occur as early in the month as possible. A similar survey was provided at the end of the month to measure the experience received. Results: 16 residents were surveyed between July 2020 and March 2021. The mean reported level of general GI knowledge at the start of the month was 4.0 and increased to 7.2 at the end of the month. TPN knowledge was rated a mean of 4.6 at the beginning of the service month and increased to a mean of 6.2 at the end of the service month. Using a pareto diagram (figure 1), it was determined that inflammatory bowel disease teaching and TPN teaching were among the most requested topics, along with short bowel syndrome and indications for endoscopy. The monthly curriculum was built to incorporate these four topics along with other highly requested teaching as early in the rotation as possible. Conclusion/Discussion: Our QI project has helped to standardize the education that all residents receive while on the GI inpatient service by identifying the most highly demanded teaching topics and prioritizing them early in each service month to meet their educational goals. Further investigation into the impact of these changes is necessary, including continued assessment of resident knowledge/comfort metrics between the start and end of each service month as well as resident satisfaction with the standardized teaching model.
-
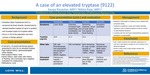
A case of an elevated tryptase
Sonya Parashar and Nikita Raje
Hereditary Alpha Tryptasemia (HαT) is an autosomal dominant disorder characterized by an elevated baseline tryptase that occurs up to 3% of the population and clinically resembles mast cell activation syndrome.
-

Antimicrobial susceptibility testing practices at cystic fibrosis care centers
Christopher M. Oermann, Claire Elson, Ellen Meier, and Megan Gripka
Background: Published data suggest a lack of correlation between antimicrobial susceptibility testing (AST) of respiratory cultures and clinical outcomes in people with cystic fibrosis (CF). Nevertheless, AST is recommended by the CF Foundation (CFF) and the Cystic Fibrosis Trust. A survey of CF center program directors was conducted to understand how susceptibility testing is performed in North American CF centers. Methods: A survey was sent by the CFF to North American CF program directors and pharmacists via a CFF email distribution list. A reminder email was sent 2 weeks later. The survey was conducted using the online platform Survey Monkey, and responses were anonymous. Results: The survey of pharmacists is to be completed. The survey was completed by 36 of the 111 (32%) program directors who opened the email invitation. Two program directors provide care for fewer than 50 people with CF (6%),13 for 50 to 100 people (36%),10 for 100 to 200 people (28%), 4 for 200 to 300 people (11%), and 7 for more than 300 people (19%). In describing current AST practices, 3 CF centers (8%) had all susceptibility testing performed by a reference microbiology laboratory rather than an internal laboratory. AST methods included automated susceptibility testing (22, 67%), disk diffusion (17, 52%), and broth/microbroth dilution (14, 42%). Regarding frequency of obtaining respiratory cultures, 34 respondents reported obtaining respiratory cultures at each ambulatory care visit (94%), and 19 respondents obtained respiratory cultures during inpatient admission (53%). Thirty-three respondents (92%) reported obtaining identification and susceptibility testing for each respiratory culture collected. The remaining 3 respondents reported variable practices for susceptibility testing based on previous culture history. When asked about ideal AST practices, 21 respondents (58%) recommended susceptibility testing on every respiratory culture. If susceptibility testing was not performed on every culture, respondents recommended susceptibility testing at least once per year (8, 50%), each time a new isolate is identified (10, 63%), and as needed for a change in symptoms or clinical status during ambulatory care visits (8, 50%). Respondents reported using susceptibility data to inform clinical decisions, including initiation of antibiotic therapy for new isolates (30, 83%), initiation of antibiotics to treat pulmonary exacerbations (31, 86%), and for individuals with multidrug-resistant infections or a history of adverse drug reactions (31, 86%). Conclusion: The association between AST and clinical outcomes in CF is unclear, but most CF centers conduct routine susceptibility testing for each isolate as part of their standard of care. Almost half of program directors believed that AST was not needed for every culture. Finally, most program directors reported using AST data to inform clinical decisions. For these reasons, additional studies are needed to assess correlations more fully between ASTand clinical outcomes, and the cost-effectiveness of AST for all isolates should be assessed.
-

COVID-19 vaccination in individuals with cystic fibrosis at a pediatric cystic fibrosis center
Christopher M. Oermann, Claire Elson, Ellen Meier, Paula Capel, Jessica Haynes, Michelle Fischer, and Stephanie Duehlmeyer
Background: Observational data suggest that most people with cystic fibrosis (PwCF) who contract COVID-19 have outcomes similar to those of the general population, although PwCF who are older or have CF-related diabetes, poor lung function, or a history of lung transplantation may be at greater risk for more severe disease. Therefore, the CF Foundation advocates for PwCF to discuss vaccination with care teams. At present, the FDA has authorized emergency use of 3 COVID-19 vaccines. ACIP/CDC guidance allows each state to determine vaccine distribution based on an individual’s exposure and risk for severe disease. This study describes the attitudes of adolescents with CF followed by Children’s Mercy Kansas City (CMKC)’s CF center whowere eligible for COVID-19 vaccination in the state of Missouri. Methods: The CMKC Cystic Fibrosis Center is located in Missouri but provides care for 234 PwCF from Missouri and Kansas. COVID-19 vaccine was received from Missouri’s and Kansas’ allocation, with distribution based on state-wide, phased, and tiered systems. Phase 1B–Tier 2 in Missouri included, among others, individuals with chronic obstructive pulmonary disease (COPD). CMKC used the inclusion of COPD to advocate for PwCF to qualify for vaccination. Phase 4 in Kansas included PwCF. CMKC was allotted doses (first and second) to be administered over 7 vaccine clinic days for all CMKC patients meeting vaccination criteria. Center staff contacted (telephone and electronic medical record messaging) and documented vaccine status of all PwCF aged 16 and older receiving care at CMKC. Results: Of the 234 individuals followed at CMKC, 56 (24%) were aged 16 and older and eligible for COVID-19 vaccination. The median age was 18.0 (16. 1–20.8), and 31 (55%) were female. Of the 56 vaccine-eligible patients, we were unable to contact 10 (18%), 18 (32%) declined, and 28 (50%) scheduled vaccination. For thosewho declined, logistical issues were most common; 2 could not travel, and 3 had scheduling conflicts. Other reasons for decliningwere mistrust in the vaccine or pandemic severity (n = 3,17%), concerns about adverse reactions (n = 1), perceived lack of susceptibility to infection (n = 1), and current SARS-COV-2 infection (n = 2); 5 (28%) individuals refused without stating a reason, and one caregiver desired consent from a minor child. Of those receiving the vaccine, 25 (89%) had received an influenza vaccination in the 2 years prior; of those that refused, 16 (89%) had received an influenza vaccination. Conclusion: Of the 56 PwCF contacted, the majority agreed to COVID-19 vaccination. Avariety of reasons were given for declining vaccination. Most troubling of these were skepticism regarding the pandemic and vaccine necessity and misconceptions about safety and efficacy. As access to SARSCoV- 2 vaccination is expanded nationally and includes younger children with CF, it will be critical for CF care center staff to proactively address issues surrounding vaccination hesitancy.
-

Delayed-Onset Anaphylactic Reaction With High Fever After Amoxicillin Oral Challenge And Negative Penicillin Skin Testing
Jordan Pitt, Paul J. Dowling, Christopher Miller, and Aarti Pandya
Introduction: Immunologic adverse drug reactions can be categorized based on Gell and Coombs’s classification system. Anaphylaxis is generally considered a type I, immediate, IgE-mediated reaction and typically occurs independent of other immunologic reactions. However, the child presented here reacted after amoxicillin challenge with features of type I and type III or IV hypersensitivity reactions. Case Description: A 12-year-old female presented for amoxicillin allergy evaluation after treatment for scarlet fever with amoxicillin. After the second dose she developed rash with varied features, fatigue, edema, and joint swelling. Labs included a persistently low C4 level, eosinophilia, normal inflammatory markers, and normal tryptase level. It was unclear if symptoms were due to infection or drug reaction, so she underwent skin testing to benzylpenicillin, benzylpenicilloyl polylysine, and ampicillin which was negative. Two hours after a graded amoxicillin oral challenge, she developed shortness of breath, diffuse erythema, and pruritus. Epinephrine was administered with symptom resolution. One hour later, she developed diffuse erythema, periorbital/lip edema, nausea, delayed capillary refill, and high fever. Epinephrine and intravenous fluids were given with symptom improvement. Tryptase level was elevated from baseline. She was admitted and discharged asymptomatic the next day. Discussion: The patient’s symptoms and elevated tryptase are consistent with delayed-onset, biphasic anaphylaxis, however the presence of high fever suggests a co-existing type III or IV hypersensitivity reaction. The literature has reported rare cases of mixed hypersensitivity drug reactions that include multiple reaction types. Recognition of this phenomenon is important when evaluating patients with adverse drug reactions involving mixed features.
-

Evaluation of the Outcomes of Trimethoprim-Sulfamethoxazole Oral Challenges in the Pediatric Population
Hannah N. Neuhaus and Salman Aljubran
Introduction: Trimethoprim-sulfamethoxazole allergy can complicate treatment for various infections. While trimethoprim-sulfamethoxazole hypersensitivity, desensitization/oral challenges are frequently reported in adults, data is limited on the outcomes/safety of oral challenges to trimethoprim-sulfamethoxazole in Pediatrics. The goal of this study was to characterize the outcomes and safety of trimethoprim-sulfamethoxazole oral challenges in Pediatrics.
Methods: An IRB-exempt retrospective chart review was performed of pediatric patients who underwent oral challenge to trimethoprim-sulfamethoxazole in Allergy Clinic over the last 12 years. We assessed characteristics including age, sex, reaction (IgE-mediated/non-IgE-mediated/indeterminate), skin testing, challenge outcome and complications to draw a conclusion regarding the overall safety of the procedure in the pediatric population.
Results: Eleven patients were identified who underwent trimethoprim-sulfamethoxazole skin testing and/or oral challenge. Two reactions were consistent with an IgE-mediated process while the remainder were non-IgE-mediated/indeterminate. Two underwent skin testing to trimethoprim-sulfamethoxazole; both negative. Ten patients underwent successful oral challenge to trimethoprim-sulfamethoxazole; the eleventh patient was lost to follow-up after skin testing.
Conclusion: Trimethoprim-sulfamethoxazole hypersensitivity is infrequently evaluated in the Pediatrics. However, trimethoprim-sulfamethoxazole is an effective antibiotic and reported allergy limits treatment for infections. Evaluation of the initial reaction is necessary, as many patients have non-IgE-mediated/indeterminate reactions. Severe cutaneous adverse reactions should be evaluated for when considering candidates for oral challenge to trimethoprim-sulfamethoxazole as oral challenge is contraindicated in these patients. Overall, this study demonstrated that oral challenge to trimethoprim-sulfamethoxazole is a safe procedure to perform in select pediatric patients and can be done safely in the outpatient setting. One limitation was small sample size.
Educational Objective: Upon completion of this session, participants should be able to discuss the overall safety of oral challenges to Bactrim in the pediatric population.
-

Impact of Early Tracheostomy on Neurodevelopmental Outcome in Infants with Severe Bronchopulmonary Dysplasia Exposed to Postnatal Steroids
Amjad Taha, Gangaram Akangire, Janelle R. Noel-Macdonnell, Tiffany Willis, and Winston Manimtim
-

Optic Disc Pit Maculopathy Leading to Vision Loss in a Pediatric Patient
Allyson Hall
This case will review optic disc pit maculopathy in children and treatments available. An emphasis in vision rehabilitation will be discussed as any visual insult during this development period can lead to long-term visual consequences.
-

Optimizing oral glucose tolerance test completion at a pediatric cystic fibrosis care center: A 10-year continuing quality improvement effort
Christopher M. Oermann, Paula Capel, Jessica Haynes, Michelle Fischer, and Jill Kohmetscher
Background: Cystic fibrosis–related diabetes (CFRD) is a common comorbidity among people with CF (PwCF). It is associated with weight loss, protein catabolism, lung function decline, and increased mortality. Nutritional status and pulmonary function begin to decline in PwCF several years before the diagnosis of CFRD. Early CFRD detection and aggressive insulin therapy have been shown to reduce the mortality gap between PwCF who have CFRD and those who do not. The Clinical Care Guidelines for Cystic Fibrosis–Related Diabetes recommend annual screening for people with CF starting at age 10 [1]. Methods: In 2011, team members at Children’s Mercy Kansas City (CMKC) embarked on a quality improvement (QI) project focused on improving oral glucose tolerance test (OGTT) completion rates in PwCF. During the initial phase of this project, QI methodology including fishbone diagrams and process flowcharts were employed to identify barriers to obtaining OGTTs. Patient education materials (English and Spanish) detailing the importance of and process for completing OGTTs were developed and distributed annually. A database for tracking PwCF who are greater than 10 years old and require OGTT was created. Weekly monitoring of upcoming appointments helped ensure that testing opportunities were not missed. Efforts were made to schedule OGTTs with annual laboratory testing to reduce phlebotomy. PwCF who wished to schedule with a local laboratory or provider were encouraged to do so and were provided with outside orders as needed. When PwCF in this group were admitted to the hospital, every attemptwas made to complete OGTTs near the end of their hospitalization. Results: Due to the lack of a standardized process and education, previous OGTT screening rates were poor: 9% in 2008, 13% in 2009, and 25% in 2010. During the first year of standard interventions (2011), the rate rose to 77%. By identifying barriers and standardizing our process, OGTT completion rates have continued to rise. In 2019 our OGTT completion rate was 92%, and in 2020—despite the COVID-19 pandemic which eliminated 3 months of testing opportunities—it was 81%. In recent years, endocrinology has partnered with the CF team in monthly CF/endocrinology “combo clinics,” which allow PwCF who have impaired glucose tolerance or CFRD to be evaluated by an endocrinology provider during their routine CF clinic visit. Conclusion: This QI project was initiated in 2011 and quality improvement work has continued to the present day. Continued education of PwCF and their families, tracking of testing, and commitment to sustained quality have allowed CMKC to attain high rates of OGTT completion. Earlier identification of impaired glucose tolerance and CFRD has allowed for earlier interventions, including dietary modifications, exercise recommendations, and endocrinology involvement in the plan of care.
-

Vancomycin AUC monitoring in individuals with cystic fibrosis at a pediatric institution
Christopher M. Oermann, Stephanie Duehlmeyer, Ellen Meier, and Claire Elson
Vancomycin AUC monitoring in individuals with cystic fibrosis at a pediatric institution S. Duehlmeyer1, C. Oermann1, E. Meier1, E. Elson1. 1Pulmonology, Children’s Mercy Kansas City, Kansas City, USA Background: Antibiotic therapy is essential for the treatment of cystic fibrosis (CF) lung infections. Methicillin-resistant Staphylococcus aureus (MRSA) infects 20% to 25% of people with CF (PwCF) and is associated with increased morbidity. Treatment of pulmonary exacerbations (PEs) often requires hospitalization including respiratory treatments and intravenous (IV) antimicrobials. IV vancomycin, which is commonly used for MRSA infections, requires serum concentration monitoring to ensure efficacy and minimize toxicity. Previous guidelines recommended trough concentrations to monitor efficacy and toxicity. Updated guidelines now recommend area under the curve (AUC) modeling as the optimal parameter for monitoring IV vancomycin. Methods: Children’s Mercy Kansas City (CMKC) changed IV vancomycin monitoring from trough to AUC/minimum inhibitory concentration (MIC) modeling on 01 May 2020 for PwCF. Two serum concentrations, a postdistributive and a trough, are obtained to estimate the AUC/MIC. A retrospective chart review collected trough monitoring data for all PwCF that received IV vancomycin at CMKC from01 January 2019 to 31 December 2019. Data for all PwCF treated with IV vancomycin after the AUC monitoring change were collected through 19 March 2021. Information on patient demographics, details of IV vancomycin therapy (dose, frequency, total exposure, nephrotoxicity), and monitoring data (serum concentrations, AUC modeling) were collected. Descriptive statistics were used to assess pre- and post-implementation data. Results: Before AUC monitoring, 25 patients received 42 courses of IV vancomycin; 14 were female (56%), and the median age was 14.02 years (4.25–20.25). Median treatment duration was 9.62 days (1.79–26.54), and median daily vancomycin exposure was 71.43 mg/kg/day (49.58–99.29). Target vancomycin trough concentration (≥15 μg/mL) was reached during 18 courses (43%). The median time to therapeutic trough was 83.58 hours (11.55–273.55) and required a median of 3 phlebotomies (1–9). Post-AUC there have been 15 courses of IV vancomycin in 8 PwCF; 5 were female (63%), and the median agewas 17.96 years (7.60–20.10). Median treatment duration was 9.52 days (5.68–14.63), and median daily vancomycin exposure was 75 mg/kg/day (48.63–92.80). All treatment courses reached target vancomycin AUC/MIC (400–600 μg/mL*h); median time to therapeutic AUC/MIC was 20.13 hours (11.6–106.12) and required a median of 3 phlebotomies (2–8). A median trough of 10 μg/mL (7–15 μg/mL) correlated with an AUC within target range. Conclusion: Changing to AUC monitoring for IV vancomycin in PwCF was not associated with a significant change in vancomycin daily exposure or duration. Fifty-seven percent more individuals achieved therapeutic targets with AUC monitoring (n = 15, 100%) than with trough monitoring (n = 18, 43%). AUC monitoring decreased time to therapeutic target by 63.45 hours. Trough concentrations of 15 μg/mL or less correlated with target AUC/MIC. A difference in nephrotoxicity was not seen. Study limitations include short postimplementation period (10 months) and small sample size. Ongoing data collection is planned.
-

A Proposal for Developing Academic Partnerships between American Clinical Institutions and NGOs
Anik Patel, Nahreen Ahmed, Alfredo Mena Lora, and Riley Jones
"Humanitarian and health-focused non-governmental organizations, such as MedGlobal, and American clinical institutions can mutually benefit from the formation of academic partnerships. MedGlobal has a longitudinal presence in ongoing humanitarian disasters that can provide rich clinical experiences for academic institutions looking to provide more diverse and equity-driven training for its residents and fellows. American institutions can provide resources, personnel with special skills and knowledge, as well as research assistance to MedGlobal and its partner sites as it continues to promote evidence-based clinical care for refugees. We propose an innovative model that addresses 3 areas of opportunities: education, research/QI, and clinical care. By regularly distributing a "menu" of opportunities dictated by needs on the ground, US academic programs can participate up to their capabilities and skill sets. These opportunities could include virtual lectures and modules, tele-health consultations, creating trainee rotations, participating in rigorous research and QI projects, holding in-person train-the-trainer sessions such as with neonatal resuscitation or ultrasound, and creating a vetted roster of American providers from partnered programs that could be deployed in the setting of acute disaster response. This model could be replicated by other NGOs working in the humanitarian space to improve education, knowledge, and clinical care for some of the most vulnerable patients in the world."
-

Assessing Early Use and Complications of Gastrostomy Blended Feeds.
James Fraser, Kristen L. Sayers, Amy L. Pierce, Beth A. Orrick, Wendy Jo Svetanoff, Tolulope A. Oyetunji MD MPH, and Shawn D. St Peter
Providers are hesitant to recommend using blended tube feeds (BF) after gastrostomy tube (GT) placement due to increased risk of bacterial contamination, nutrition inadequacy, tube blockages, and lack of data addressing clinical outcomes. Caregivers often feel that BF are more natural, better tolerated, and more cost-effective. We studied early use of BF, potential complications, and satisfaction among caregivers.
-

Descriptive Study of the Safety Behaviors and Attitudes of Portable Pool Owners
Kristyn Jeffries, Kathy W. Monroe, Alicia Webb, Kristin L. Chancellor, Justina C. Goldman, and David C. Schwebel
Background Drowning is the leading cause of injury death for children 1-4 years old and the second leading cause for children 5-9 years old. Most prior epidemiology work has focused on submersions in below-ground swimming pools and natural bodies of water. Portable pools pose a new and emerging risk for drowning due to their affordability, convenience, and easy assembly. Successful drowning prevention consumer products, such as 4-sided fencing, may prove more difficult to implement with portable pools, and currently are not marketed for such use. Furthermore, parental perceptions and knowledge of drowning risks associated with portable pools has not yet been well studied.
Methods We performed a prospective study of caregivers to children aged 9 months to 6 years in an urban pediatric emergency department during summer 2021. Enrolled caregivers were given a QR code that directed them to complete a self-administered questionnaire on their mobile device. Survey questions assessed the caregivers’ access to portable pools and their safety behaviors and attitudes related to portable pools. Frequencies of portable pool ownership, caregivers’ safety practices while using them, and caregivers’ behavioral perceptions were calculated.
Results Of the 85 caregivers enrolled in the study, 54% reported either owning or having access to a portable pool. Of the subset who owned portable pools, a majority (n=23/28) bought their portable pool in 2021, but only 28% (n=8/28) used any safety products with their pool and only 10% had previously enrolled their child in formal swim lessons. The primary reasons portable pool owners did not use safety products included perceived lack of necessity of such products for portable pools and confidence in close supervision while their child is swimming. While all caregivers (n=85/85) responded they would always watch their child in the shallow end of a below-ground pool, 14% (n=12/85) of caregivers responded they would only watch their child intermittently while in a portable pool. Over 48% (n=41/85) of caregivers thought they would hear their child if he/she was drowning in a portable pool.
Conclusions Parents may underestimate the risk associated with portable pools, which could contribute to young children’s risk of drowning in these pools. These results provide insights that could be used in the development of drowning prevention messaging and the development of prevention strategies specifically targeting portable pool users.
-

Pharmacogenetic Testing In Patients with Autism Spectrum Disorder Evaluated in a Pediatric Precision Medicine Clinic
Rachel Goodson, Cy Nadler, Jennifer A. Wagner, Sarah Soden, Sarah Nyp, and Tracy L. Sandritter
Pharmacogenetic Testing In Patients with Autism Spectrum Disorder Evaluated in a Pediatric Precision Medicine Clinic Purpose The purpose of this study is to investigate the demographic and presentation profiles of children with autism spectrum disorder (ASD) who present for evaluation in a pediatric precision medicine clinic. Methods: This retrospective, observational cohort study utilized data extracted from a pediatric precision medicine clinic database between 2010 and 2021 with recorded ICD9/10 codes of Autism Spectrum Disorder, Autistic Disorder, Pervasive Developmental Disorder, or Asperger’s Syndrome. Extracted variables included demographic data, presenting medication regimens and concerns to be addressed by precision medicine. Results: A sample of 202 patients was identified (see Table 1). Patients referred for precision medicine services were primarily due to poor medication response (64.8%) and/or adverse drug reactions (48.5%). Referrals were made by subspecialists (78.2%), primary care providers (16.3%), and via self-referral (4.95%). At presentation to the clinic, patients were already prescribed between 1-10 medications (Mean = 6.15, Median 5; see Figure 1). Medications with indication commonly used for sleep, gastrointestinal disorders, and psychiatric/behavioral disorders were among the most common medications taken at the time of evaluation (see Figure 2). At time of presentation to the clinic, males and females did not differ in terms of age (t= 1.22, p = 0.22) or number of medications taken (t = 0.994, p = 0.323). Age was also not significantly associated with number of medications (F = 0.277, p = 0.527). Conclusions: Youth with ASD presenting for precision medicine consultation experienced notable degrees of polypharmacy, with no clear differences associated with sex or age. Trends may emerge with the addition of a typically developing control group, and the robustness of associations must be evaluated in samples drawn from a wider variety of practice settings. While these findings are primarily descriptive, the data fill a critical gap regarding the characteristics of youth with ASD referred for precision medicine. Few dedicated precision medicine clinics exist, yet this service is increasingly recommended for youth with autism due to higher rates of adverse drug reactions and clinical nonresponse. More research is needed to establish how precision medicine fits within existing evidence-based guidelines and can most effectively serve this population.
-

Racial Disparities in Testicular Torsion
Kayla B. Briggs, Obiyo O. Osuchukwu, Chris E. Roberts, James Fraser, Wendy Jo Svetanoff, Tolulope A. Oyetunji, and Hanna Alemayehu
Racial Disparities in Testicular Torsion Introduction: Testicular torsion (TT) is a surgical emergency requiring prompt intervention to preserve testicular function. Race and insurance status are thought to be associated with higher rates of gonadal loss; however, reports in the literature are conflicting. We sought to determine the effect of race on the treatment and outcomes of testicular torsion. Methods: Following IRB approval, a retrospective review was conducted of patients <18 years of age who presented to 2 institutions>(hereby referred to as H1 and H2) with acute scrotal pain between December 2017 and September 2019. Demographic data, clinical history, imaging results, diagnosis, and surgical outcomes were recorded. Social vulnerability index (SVI), as determined by zip code, was obtained from the Centers for Disease Control and dichotomized using the 75th percentile. Higher SVI denotes increased social vulnerability. Primary outcome was diagnosis of TT. Secondary outcomes included orchiectomy rates. A p-value <0.05 was considered significant. Results: A total of 515 patients (H1 85%, H2 15%) were included in the final analysis. There were no difference in median age, BMI, TT diagnosis and orchiectomy rate between the two institutions. H2 treated more black patients (43% vs. 14%, p=<0.01) and patients with public insurance (57% vs. 41%, p=0.03) compared to H1. In multivariate analysis, older age was associated with TT (median age TT 14.12 years [12.13,15.69]) vs. no TT 9.86 years [5,13.05], OR 1.35, 95% CI 1.18-1.55, p=<0.01). Black patients were ~4 times more likely (OR 4.05, 95% CI 2.13-7.69, p=<0.01) than white patients to be diagnosed with TT when controlled for dichotomized SVI, insurance, and age. In the same model, Hispanic patients were ~2 times more likely (OR 2.20, 95% CI 1.10-4.40, p=0.03) to be diagnosed with TT when compared to white patients. Despite more black and Hispanic patients having dichotomized SVI >75th percentile than white patients (70% and 82%, respectively vs. 16%, p=<0.01), dichotomized SVI was not found to be associated with higher rates of TT or orchiectomy, respectively. Conclusion: At the two centers, more black and Hispanic children had SVI >75th percentile, however, when controlling for this in multivariate analysis, they were significant more likely to be diagnosed with testicular torsion. Conversely, there was no difference in orchiectomy rate between races.
-

Severe diastolic dysfunction following prolonged extracorporeal membrane oxygenation in a pediatric burn patient.
Cara Holton, Johanna I. Orrick, Igor Areinamo, and Jenna Miller
A previously healthy 3-year-old female was admitted following a 22% TBSA scald burn. She was initially hemodynamically stable on room air. However, one week into hospitalization she developed ARDS with catecholamine-refractory shock requiring VA-ECMO. She was enterovirus positive, grew MRSA in respiratory cultures and was treated with prolonged antibiotics. The patient spent 26 days on VA-ECMO followed by 61 days on VV- ECMO after failing decannulation due to refractory hypoxia. She developed anuric renal failure requiring CRRT during her second ECMO course. Following VV-ECMO decannulation, she required mechanical ventilation with high settings and had severe recurrent pulmonary hemorrhage requiring FFP, platelets and inhaled TXA. She had coronary dilation on CT imaging but was COVID-19 antibody negative. Serial echocardiograms demonstrated moderate LV dilation with normal systolic function. It was difficult to assess her diastolic function by echo, but with clinical concern for dysfunction she was started on milrinone. She underwent cardiac catheterization due to pulmonary bleeding and concerns for pulmonary hypertension. She had severely elevated biventricular filling pressures (RVEDp of 38 and LVEDp of 55) indicative of diastolic dysfunction. She had a high baseline cardiac index and normal PVR on milrinone and sildenafil. She also had significant AP collateral burden requiring coiling. Following this procedure her pulmonary hemorrhage resolved but her pulmonary mechanics did not improve. She continued to have multi-system organ failure with cardiac dysfunction, respiratory and renal failure. Her family did not wish to pursue organ transplantation and chose to redirect her care. This case is remarkable for several reasons. While large burns are known to produce an inflammatory response with cardiac dysfunction (1, 2), typically the degree of inflammation is proportional to the size of the burn and occurs early (3). This patient had a smaller TBSA burn that did not require surgery, yet she developed profound respiratory failure and shock requiring ECMO. During her hospitalization and 87 days on ECMO, the patient developed severe diastolic heart failure, AP collateral burden and coronary ectasia. This case demonstrates the utility of a diagnostic cardiac catheterization to evaluate for hemodynamic abnormalities after prolonged ECMO support, especially when echocardiogram is unrevealing. It is impossible to say whether these findings were a result of her prolonged ECMO runs, her burn physiologic state, or potentially a synergistic combination of the two. Additionally, while “long run” ECMO is becoming more common, little is known about the long-term cardiovascular effects of ECMO physiology. We report this case to encourage others to share cardiovascular complications after ECMO runs greater than 21 days.
-

Short and Long Term Outcomes of Using Cryoablation for Post-operative Pain Control in Patients After Pectus Excavatum Repair
James Fraser, Kayla B. Briggs, Wendy Jo Svetanoff, David Juang, Pablo Aguayo, Jason D. Fraser, Charles L. Snyder, Tolulope A. Oyetunji, and Shawn D. St. Peter MD
Background: Previous prospective trials have demonstrated that intercostal cryoablation reduces length of stay and postoperative opioid consumption compared with thoracic epidural and patient controlled analgesia (PCA) modalities. We report the findings of a 3-year prospective, observational study to elucidate long-term pain control, symptoms, and complications with attention to postoperative short and long-term pain control associated with the cryoablation technique.
Methods: Following IRB approval, we prospectively collected data on patients who underwent bar placement for pectus excavatum with thoracoscopic intercostal cryoablation by six surgeons at our institution from 2017 to 2021. Patients and their parents completed surveys regarding pain scores, narcotic and non-narcotic pain medication usage, and limitations to activity beginning on the day of surgery for up to 10 days, with a supplementary survey on the day of discharge to evaluate pain and associated symptoms. Surveys were administered at two-week and three-month follow-up appointments addressing pain control, symptoms, and limitations to activity. Retrospective review of chart data was performed to identify the number of emergency department visits, phone calls to the outpatient surgery office, and requirement for additional pain medication.
Results: 110 patients were included in the analysis; 90% were male with a median age of 15.8 years [14.6, 16.7]. The median length of stay was 25.6 hours [22.3, 31.7]. Forty-eight patients (44%) completed the discharge survey; sharp pain and pressure on the first night of surgery were the most described pain characteristics, with sharp pain being the worst symptom reported most frequently in the middle of the chest. (Table 1) On postoperative follow-up, 55% of patients reported tolerable residual pain at two weeks and 41% at three months, with a median pain score of 3 at each follow-up interval and 25% of survey respondents requiring intermittent non-narcotic pain medication at three months. There were 18 (16%) ED visits by two-week follow-up, resulting in 3 readmissions for inadequate pain control: two on postoperative day two and one on postoperative day five. By three-month follow-up, there were 65 calls to the surgery clinic, most commonly for persistent pain and frequent popping sensation with movement, and no additional patients required readmission for pain control within this longer interval. (Table 2)
Conclusion: Although cryoablation is an excellent pain control modality to attenuate the acute insult of bar placement, these data suggest that patients underreport functional symptoms and experience more frequent discomfort and alteration of activities of daily living than perceived by providers. Prospective validation is necessary to examine the nature of specific symptoms, duration, and impact on the patient’s quality of life. -

Improving Skin and Soft Tissue Antibiotic Duration Concordance with National Guidelines in Pediatric Urgent Care Clinics
Megan Hamner, Amanda Nedved, Holly Austin, Donna Wyly, Alaina N. Burns, Diana King, Brian Lee, and Rana El Feghaly
Introduction: Skin and soft tissue infections (SSTIs) are the second most common diagnosis leading to pediatric antibiotic prescriptions in the outpatient setting after respiratory diagnoses. Children with SSTIs often receive >7 days of antibiotics, although current guidelines recommend 5-7 days for most diagnoses. At CMH urgent care clinics (UCCs), only 58% patients received the recommended 5-7 days of antibiotics. We aimed to increase the percentage of patients receiving 5-7 days of oral antibiotics for SSTIs from 58% to 75% by December 31st, 2021. Methods: We formed a multidisciplinary team in April 2020. A provider survey assessed factors influencing prescribing habits. We completed cause-and-effect analyses and developed a driver diagram (Figure 1). Interventions were chosen based on the potential for highest impact and lowest effort. Our first Plan-Do-Study-Act (PDSA) cycle provided an update on current guidelines for UCC providers. The second PDSA cycle updated prescription sentences in the electronic health record (EHR) and organized them from shortest to longest duration. The third PDSA cycle provided a project update via email to UCC providers. Our outcome measure is the percentage of patients receiving 5-7 days of antibiotics for SSTIs. Process measure is the number of updated prescriptions used. Balancing measure is the number of patients returning for SSTI within 14 days of their visit. Results are displayed using a run chart. Results: After initiation of the project in April 2020, the percentage of patients receiving 5-7 days of antibiotics increased to 68% (Figure 2). This percentage increased to our goal of 75% after the 1st PDSA cycle (October-December 2020), 80% following the second PDSA cycle in February 2021, and 90% following the third PDSA cycle in April 2021. There was no change in balancing measure numbers. Conclusion: Prior to our project, only 58% of children seen in CMH UCCs for SSTIs received the recommended antibiotic duration. By addressing the primary drivers uncovered through QI methodology, we surpassed our goal of 75%. Additional PDSA cycles are planned along with expansion to other departments. This work will allow us to expand antibiotic stewardship efforts to other infectious diagnoses as well.
-

Reconsidering Perioperative Antibiotic Use in Elective Laparoscopic Cholecystectomy
Kayla B. Briggs, James Fraser, Wendy Jo Svetanoff, Charles L. Snyder, Pablo Aguayo, David Juang, Rebecca M. Rentea, Jason D. Fraser, Shawn D. St. Peter MD, and Tolulope A. Oyetunji
Introduction: Prophylactic preoperative antibiotics (PPA) are questionable in cases with a low rate of surgical site infection (SSI). We report institutional PPA usage and SSI rates after elective laparoscopic cholecystectomy in a children’s hospital. Methods: Children <18 years old who underwent outpatient laparoscopic cholecystectomy between 7>/2010 and 8/2020 were included. SSI was defined as clinical signs of infection, requiring antibiotics, within 30 days of surgery. Results: 502 patients met inclusion criteria; 50% were pre-operatively diagnosed with symptomatic cholelithiasis, 47% biliary dyskinesia, 2% hyperkinetic gallbladder, and 1% gallbladder polyp(s). The majority were female (78%) and Caucasian (80%). 60% (n=301) of patients received PPA while 40% (n=201) did not; 1.3% (n=4) of those who received PPA developed SSI compared to 5.5% (n=11) of those who did not (p=0.01). Though PPA use was associated with an 84% reduction in risk of SSI on multivariate analysis (p=0.01), all SSIs were superficial. One child required readmission for intravenous antibiotics while the remainder were treated with outpatient antibiotics. Gender, age, BMI, ethnicity, and preoperative diagnosis did not influence the likelihood of receiving PPA (Table 1). Conclusion: Given the relatively low morbidity of the superficial SSI, conservative use of PPA should be carefully considered in outpatient laparoscopic cholecystectomy to avoid contributing to antibiotic-related complications.
-

Challenges in Echocardiographic Diagnosis of Corrected Malposition of Great Arteries: The Segmental Approach coming Handy
Amulya Buddhavarapu, Anmol Goyal, Sanket Shah, Nitin Madan, Hayley S. Hancock, and Maria Kiaffas
Clinical Presentation
Two cases of {S,D,L} anatomically corrected malposition of great arteries (ACMGA) are presented with differences in conal anatomy. Case 1: A fetal echocardiogram (echo) performed at 28 weeks gestation due to multiple anomalies revealed atrial situs solitus, D-loop ventricles, a large conoventricular septal defect (VSD) and an overriding, anterior and leftward aorta. The diagnosis of double outlet right ventricle (DORV) vs ACGMA was entertained. Postnatal echo revealed {S,D,L} segmental anatomy with ventriculoarterial concordance consistent with ACGMA and a muscular VSD. Case 2: A 3-week-old boy presented to clinic for a murmur evaluation with no associated cardiac symptoms. Transthoracic echocardiogram revealed {S,D,L} ACGMA and a small membranous VSD.
Imaging Findings
Echocardiographic subcostal, parasternal and suprasternal sweeps help diagnose ACGMA by delineating ventriculoarterial alignment, ventricular and outflow relations and conal anatomy. Case 1, a rare ACMGA type, posed the most diagnostic challenges. A more anterior rotation of the left ventricle, horizontal orientation of the ventricular septum due to absence of a sub-pulmonary conus, in combination with an elongated subaortic conus led to the misconception of an overriding aorta and DORV prenatally. Pulmonary to tricuspid valve fibrous continuity was present. The unusual position of the aortic valve resulted in an elongated curvature of a left aortic arch, coursing from anterior and right towards the left of the trachea. Case 2, the most typical type of {S,D,L} ACGM, had the usual anatomic characteristics of bilateral sub-arterial conus and parallel outflow tracts. In both cases cardiac magnetic resonance imaging was performed for evaluation of the Qp/Qs caused by the VSD and confirmed the diagnosis of ACGMA.
Roles of Imaging in Patient Care
Accurate prenatal diagnosis of ACMGA is essential for appropriate counseling and postnatal management. Postnatally, standard echocardiographic views and multimodality imaging will elucidate ventriculoarterial connections, conal anatomy, and severity of associated anomalies.
Discussion
ACMGA is a rare congenital heart disease occurring from failure of involution and rightward rotation of the subaortic conus resulting to a parallel spatial relationship of the great arteries while maintaining ventriculo-arterial concordance. Subtypes include {S,D,L} (most common, usually with bilateral conus) and {I,L,D} with normal, and {S,L,D} and {I,D,L} with transposition physiology. Identifying the segmental anatomy and relations will result in accurate diagnosis of this rare entity.
-

Correlation between strain and weight status in infants with a univentricular hear
Amulya Buddhavarapu, Mathew Warren, Lori Erickson, Christopher Mathis, Whitney Haas, and Daniel Forsha
Background
Infants with univentricular physiology are at risk of poor weight gain and reduced ventricular function, both of which have been independently associated with worse outcomes. Since nutritional status has been correlated to ventricular function in other populations, we evaluated the relationship between nutritional status and ventricular function including speckle-tracking strain during this period.
Methods
Thirty term infants (median age 55 days, 13 females) with univentricular physiology prior to stage II palliation were included with data obtained at the time of their initial hospital discharge. Ventricular function was quantified using 2D global longitudinal strain (GLS) and strain rate, analyzed from an apical “4-chamber” view (TomtecCPA 2.31). Ventricular myocardium was tracked along the dominant walls producing systolic ejection-- the lateral and septal walls of the dominant ventricle in cases of a single RV or LV and both the lateral LV and RV walls in the presence of an unrestrictive ventricular septal defect and biventricular mass, such as an unbalanced AV septal defect. Statistical analysis using SPSS reported the median with interquartile range (IQR) and utilized Spearman or Pearson correlation testing as appropriate (P < 0.05 significant).
Results
Stage I palliation was performed in 29/30 (14 Norwood, 8 BT shunt, 5 PA bands, and 2 hybrids). GLS correlated with weight for age z-score (WAZ) scores (r= -0.45, p= 0.01) and trended toward correlation with weight for length z-score (r=-0.31, p =0.09) in this small study. Multivariate regression model using GLS as the dependent variable against WAZ score and atrioventricular regurgitation revealed an independent association between GLS and WAZ score (p=0.03) while the association of GLS with atrioventricular valve regurgitation lost significance (p=0.06). On ANOVA analysis of GLS based on ventricular morphology, GLS was diminished in the single RV subgroup [median -13.1% IQR (-15, -10.7)] compared to GLS in single LV [-17.2% (-21, -12.5)] and biventricular [-17.2% (-18.1, -14)] subgroups (p=0.043).
Conclusion
Lower WAZ-scores at the time of neonatal discharge are associated with lower GLS. Systemic right ventricles have lower GLS.
-

Longitudinal analysis of myocardial function using strain in patients receiving cardiotoxic chemotherapy
Anmol Goyal, Amulya Buddhavarapu, Kayla Simpson, Nataliya Kibiryeva, Wendy Hein, Joy M. Fulbright, and Sanket Shah
Background:
Chemotherapy-related cardiotoxicity (CTRC) is associated with significant morbidity and mortality in long-term cancer survivors. Left ventricular [LV] Global longitudinal strain (GLS) is a sensitive parameter that can be used for earlier detection of contractile function changes in these patients. Recent literature suggested certain genotypes may influence CTRC. Our goal was to assess longitudinal myocardial function and identify any correlation between certain genetic variations and LV function regarding CTRC in our pediatric population.
Methods:
50 subjects ≥10 years of age who have survived >2 years after completion of cancer treatment were enrolled out of which 29 subjects agreed for genetic analysis and follow-up evaluation of echocardiograms. Echocardiographic data from these 29 subjects was reviewed. Apical 4 chamber and short axis at the level of papillary muscles were used for area-length 2D Ejection fraction (EF) [bullet method], and apical 4 chamber image was used for GLS. GLS was performed by using speckle tracing retrospectively with 2D STE offline analysis software (4D LV-Analysis 3) developed by TomTec Imaging Systems. Seventeen of these 29 patients had longitudinal echocardiographic data available for serial measurement of their EF and GLS. GLS ≤-18% was considered normal. Paired t-test analysis was performed for these patients with follow-up data available using SPSS statistics 27.0. All 29 patients underwent whole exome sequencing for genetic polymorphism, the results of which are pending at the time of submitting this abstract.
Results:
Baseline GLS was normal in 28/29 patients (96.5%). Mean GLS was -21.71% ± 2.36 %. Mean EF was 60.1% ± 5.4%. Mean follow-up duration was 4.1 years [range 2.2-6.5 years]. At follow-up evaluation, the mean reduction of strain was 1.4 % [standard deviation (SD) of 2.1, p = 0.015] and reduction of EF was 1% [SD of 5.6, p=0.45]. Longitudinal data in 17 patients showed a decrease in GLS by >2% in 47 % of patients, however, only 11.7% of the patients had a concomitant significant decrease in EF of ≥5%.
Conclusions:
In this cohort of pediatric cancer patients, clinically all were asymptomatic; in New York Heart Association Heart failure class 1. With a mean follow-up period of 4 years, there was statistically significant reduction in GLS while EF essentially remained stable. GLS can be a more sensitive marker to assess longitudinal ventricular function than EF and can be a valuable tool in risk-stratifying patient receiving cardiotoxic chemotherapy. Additional multi-center longitudinal studies evaluating the long-term prognostic implications of reduced LV GLS in this population are essential.
-

Transient Tricuspid Valvulitis: Another Brief Casualty of COVID-19 in Children
Amulya Buddhavarapu, Girish S. Shirali, Stephen Kaine, and Doaa Aly
Clinical Presentation:
We discuss 3 patients, 8-10 years old, with significant tricuspid valve dysfunction during initial days of admission for multi-system inflammatory syndrome in children (MIS-C) associated with coronavirus 2019 (COVID-19) infection.
All 3 patients had COVID antibodies and presented in uncompensated shock needing aggressive fluid resuscitation and vasoactive support. Elevated acute inflammatory markers, acute kidney injury (2/3 patients), troponin leak and repolarization abnormality on ECG were present on admission and resolved by discharge. All were treated with intravenous immunoglobulin (IVIG) infusion, high-dose steroids and prophylactic low molecular weight heparin. They were discharged home on aspirin and steroid taper.
All patients had depressed left ventricular systolic function with LVEF of 38-52% and trivial to mild mitral regurgitation. Following fluid resuscitation and administration of IVIG, all patients developed moderate to severe, new-onset tricuspid valve regurgitation (TR) with failure of leaflet coaptation and normal tricuspid regurgitation velocities, with a TR vena contracta of 6-9 mm. Right ventricular (RV) systolic function as measured by fraction area change and TAPSE ranged from low normal to moderately decreased. RV size and tricuspid annular diameter Z score was normal for all patients.
All 3 patients responded to diuresis and fluid restriction and had mild TR at discharge.
Imaging Findings:
Our patients demonstrated an interesting pattern of early, acute onset, moderate to severe tricuspid valve regurgitation, with a wide gap of non-coaptation between the septal and anterior tricuspid valve leaflets leading to a broad central jet of TR. The degree of TR was disproportionate to the degree of RV systolic dysfunction or annular dilatation.
Role of Imaging in Patient Care:
We postulate that the etiology of tricuspid valve dysfunction is a combination of valvulitis / papillary muscle dysfunction, RV diastolic dysfunction and volume overload due to fluid resuscitation and IVIG. The frequency of these findings points to the need for judicious volume resuscitation and slower IVIG infusions in MIS-C.
Summary/Discussion Points:
TR associated with MIS-C in the pediatric population appears to be transient, and responsive to alterations in the patient’s volume status and inflammatory state. This is in contrast to adults, in whom TR with RV dysfunction has been identified as a predictor of mortality.
-
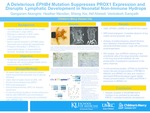
A Deleterious EPHB4 Mutation Suppresses PROX1 Expression and Disrupts Lymphatic Development in Neonatal Non-immune Hydrops
Gangaram Akangire, Heather Menden, Sheng Xia, Atif Ahmed, and Venkatesh Sampath
Background: Non-immune hydrops fetalis is often a fatal condition and in 20% of cases related to lymphatic anomalies. Maldevelopment of lymphatic valves, atretic or absence of central lymphatic vessels has been described in hydrops fetalis, but the genetic basis of these anomalies remains undefined. Recent reports suggest that Ephrin type B receptor 4 (EPHB4) gene has a significant role in embryonic development of lymphatic system. To test the hypothesis that EPHB4 mutations can cause hydrops fetalis, we combined whole exome sequencing (WES) with functional and pathological analysis of an infant who succumbed to neonatal hydrops.
Objective: To discover the possible mechanism of non-immune hydrops in EPHB4 variant by WES, histopathologic analysis and in vitro functional analysis of genetic mutation in human lung endothelial cells (HLEC).
Design/Methods: 35-week, 4.11kg male infant developed hydrops prenatally requiring multiple thoracentesis postnatally due to bilateral chylous pleural effusions and ascites, and eventually succumbed to infection and immunodeficiency from T-lymphocyte depletion. WES was performed to identify genetic causes of non-immune hydrops. Immunohistochemistry (IHC) was performed on autopsy specimens of lung and intestinal tissue. In vitro functional analysis was done using HLEC, and immunoblotting used of investigating signaling events.
Results: Magnetic resonance imaging (MRI) lymphangiogram showed complete absence of central lymphatic ducts (Figure 1). WES showed a rare heterozygous missense mutation in EPHB4 (p.Ala700Thr) that was maternally inherited. Autopsy revealed pulmonary lymphangiectasia, depletion of lymphoid tissue, and staphylococcus aureus in spleen. IHC showed loss of PROX1 expression (prospero homeobox protein 1) in large lymphatic channels in lung and small intestinal villi (Figure 2). In vitrofunctional studies showed the EPHB4 mutation resulted in loss of phosphorylation, decreased ERK phosphorylation and suppressed PROX1 expression, necessary for lymphatic valve development (Figure 3).
Conclusion(s): We report a novel case of fatal non-immune hydrops with lymphatic anomalies associated with an EPHB4functional mutation that suppresses its phosphorylation and PROX1 expression. This report highlights the importance of screening for EPHB4 variant in infants with the diagnosis of non-immune hydrops fetalis and lymphatic anomalies. This discovery will trigger further studies to find genetic basis of non-immune hydrops and novel therapies for this fatal disease.Presented at the 2021 PAS Virtual Conference



