These posters have been presented at meetings in Children's Mercy and around the world. They represent research that was done at the time they were created, and may not represent medical knowledge or practice as it exists at the time viewers access these posters.
-

Incidental Diagnosis of Dual Arterial Supply of the Right Lower Lobe
Christopher Mathis, Jay Crockett, and Maria Kiaffas
Description of Clinical Presentation: A 15 year old male with a 2 week history of fever and abdominal pain had an abdominal/pelvic MRI demonstrating osteomyelitis of his right hip. Incidentally an anomalous vessel arising from the abdominal aorta and coursing to the vasculature of the lower right lung lobe was identified and he was referred to cardiology for further evaluation. He is an athlete with no history of cardiac or respiratory symptoms and his cardiac physical examination was within normal limits. Diagnostic Techniques and Their Most Important Findings: An echocardiogram was initially obtained; imaging was difficult due to suboptimal acoustic windows and revealed normal intracardiac anatomy and normal ventricular size and systolic function. Detailed profile of the right pulmonary venous connections was not feasible and an abnormal flow close to the inferior vena directed towards the thoracic cavity was seen. The suspicion of an anomaly involving the right lung vasculature was raised and a cardiac MRI (CMRI) was obtained in order to better assess cardiovascular anatomy and calculate Qp:Qs. CMRI revealed an anomalous systemic arterial supply of a small portion of the right lower lobe without pulmonary sequestration. The artery originated from the celiac trunk with proximal narrowing of the vessel close to its origin and post-stenotic dilation. There was normal right pulmonary artery arborization and supply to this segment, indicating dual arterial supply. Qp:Qs was normal (1.03) with normal atrial and ventricular volumes indicating minimal extracardiac shunt. Learning Points from this Case: Incidental MR imaging findings are not uncommon and further imaging work-up as well as management should be individualized. In this case a systemic arterial supply to the right lower lung was inadvertently identified and further imaging revealed no hemodynamic burden associated with it. Various case reports address similar incidental discoveries, usually associated with work-up for hemoptysis, congenital heart disease and often associated with lung sequestration. Ligation or embolization of the systemic feeding vessel to the lung due to risk of hemoptysis is often undertaken. In the case of our patient, the morphology of the feeding vessel in combination with normal lung appearance, normal Qp:Qs, and lack of symptoms led to a consensus to not intervene but to observe with regular follow-up.
-

An Unexpected Global Health Experience in Manila
Susan McAnany
Describes her experience in the NICU of the Fabella Memorial Hospital in Manila, Philippines.
-

Baylor International Pediatric AIDS Initiative (BIPAI): Maseru, Lesotho
Whitney J. Cameron
Describes her experience working in Maseru, Lesotho.
-

FIT Clinical Decision-Making: Brain abscess in a nonfenestrated Fontan patient
Bethany Runkel, Natalie Shwaish, Geetha Raghuveer, and William Drake
-

FIT Clinical Decision-Making: Isolated polymorphic ventricular tachycardia in a pediatric patient: an unusual presentation of acute mycocarditis
Natalie S. Shwaish, Bethany Runkel, and Lindsey Malloy-Walton
-

FIT Clinical Decision-Making: Uhl's anomaly: an uncommon cause of fetal cardiomegaly
Bethany Runkel, Atif Ahmed, Tara Swanson, and Maria Kiaffas
-

FIT Clinical Decision-Making Unusual echocardiographic findings of myocarditis mimicking an aortic runoff lesion
Sarah Studyvin, Christine Symes, Barbara A. Pahud, and Nitin Madan
-

Global Health Elective in Santiago Atitlan, Guatemala
Sarah Greenberg
Describes her experience working in Hospitalito Atitlan in Santiago Atitlan, Guatemala.
-

Global Health Immersive Elective in the Philippines
Lisa Godfrey
Describes her experiences working at Fabella Memorial NICU and the Philippines General Hospital.
-

Medicine and Culture Abroad: Lago de Atitlan, Guatemala
Micah Helton
Describes her experience working alongside a Guatemalan General Practice Physician in Lago de Atitlan, Guatemala.
-

Philippines: An Int-ERUPTED Experience
Susamita Kesh
Describes her experience working in the NICU of the Fabella Memorial Hospital in Philippines.
-

Two Months of Global Health in Maseru, Lesotho
Rachel Hildebrand
Describes her experience working with infants and children at the Center of Excellence and Adolescents at Queen Mamohato Memorial Hospital in Maseru, Lesotho.
-

How to use Peanut IgE Levels to Predict Challenge Outcomes in the Pediatric Population
Nalin U.G., Jay Portnoy, Jodi Shroba, and Salman Aljubran
Introduction: The accepted clinical practice is to consider oral challenge when peanut IgE levels are 2.0 kUA/L or less in patients with a history of a major reaction or less than 5.0 kUA/L in patients with only sensitization. Certain populations are predisposed to having increased IgE levels, and these patients are often not offered challenges due to elevated numbers.
Methods: We reviewed unidentified patients information from January 2017 to July 2019 on peanut IgE levels and oral challenge outcomes through REDCap database. A ROC using SPSS from IBM was used and the points from the ROC curve were used to make an exponential regression curve. Since the likelihood ratio is the derivative of the ROC, the derivate of the graph was obtained.
Results: There were 106 peanut challenges (56 passed and 47 failed). The ROC points created an exponential regression of 0.417x ˇ 2 + 0.2943x + 0.0083 with an r value of 0.9072. The area under the curve was 0.702 (CI 0.601-0.803). The derivative was 0.834x+0.2943, which represents the likelihood ratio. Thus, solving the equation IgE ¼ (likelihood ratio-0.2943)/0.834.
Conclusion: It is important to remember that every patient is different, and the risk associated with oral challenge varies based on the clinical history. Using the likelihood ratio as opposed to a set threshold IgE level could enable us to better predict the possibility of a reaction with a more dynamic IgE cutoff. By using the patientspecific likelihood ratio, we were able to find an equation to allow us to calculate more meaningful IgE cutoff.
-
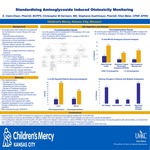
Standardizing Aminoglycoside Induced Ototoxicity Monitoring
Claire Elson, Christopher M. Oermann, Stephanie Duehlmeyer, and Ellen Meier
Aminoglycoside (AG) antibiotics are essential for the treatment of cystic fibrosis (CF) lung infections. Pseudomonas aeruginosa. Nontuberculous mycobacteria. Monitoring is critical secondary to potential nephrotoxicity and ototoxicity. Children’s Mercy Kansas City (CMKC), standardized nephrotoxicity monitoring in 2016. Observed variable ototoxicity monitoring practices. Prevalence of ototoxicity, 2016 CFF Patient Registry, 1.1% in pediatric patients (less than or equal to 18 years). 2.2% in pediatric and adult population. National Institute of Deafness and Other Communication Disorders, 13% in US population equal to or less than 12 years old. A standardized AG induced ototoxicity monitoring algorithm (AIOA) was developed and implemented at CMKC in 2017.
-
Teaching Skills for Self Sufficiency: Health Management for Patients with Disabilities and Chronic Health Conditions
Teresa M. Hickam and Kathy Smith
Research shows patients who develop self-health management skills are able to translate these skills in other life domains such as higher education, social interaction and employment. Persons with chronic health conditions or disabilities often face challenges securing employment which in turn impacts self sufficiency and long-term health. The poster focuses on two programs at Children's Mercy serving as key building blocks for adolescents to manage their lives.
-
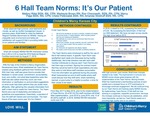
6 Hall Team Norms: It's Our Patient
Mallory Rittel, Markeyta Brown, Ron Chenoweth, Marcy Page, Chelsi Peterzalek, and Amanda Woldruff
Aim Statement
6 Hall will increase NDNQI RN-RN interaction scores from 5.06 to 5.45 to meet the 2019 National Magnet Facilities benchmark b August 1, 2019.
6 Hall Team Norms
- We strive for excellence: our work is complex, mistakes will happen.
- We provide timely (<1>week) feedback, which includes positive, learning and interpersonal feedback.
- We celebrate as a team and our environment feels like every individual matters.
- When trust is broken, we ask ourselves: how did I contribute? What can I do to make it better? We are careful in not making assumptions.
- Our behaviors are supportive and display respect.
- We create a work environment that feels consistently awesome.
-

A Multifaceted Approach to Improve Quarterly Visit Rates at a Pediatric Cystic Fibrosis Care Center
Paula Capel, Jessica Banks, Micaela McKenna, Ashley Andrews, and Christopher M. Oermann
Standard quality improvement methodology was used to improve quarterly visit rates among cystic fibrosis patients at Children's Mercy Kansas City Cystic Fibrosis Center.
- A family-centered, team-based approach was adopted
- A change in culture led to sustained improvement
Improved quarterly visit rates should drive improvement in outcomes including pulmonary function and nutritional status.
-
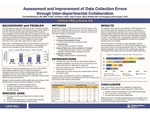
Assessment and Improvement of Data Collection Errors Through Inter-departmental Collaboration
Charlott Williams, Kelli L. Behr, Mary Moffatt, and Rangaraj Selvarangan
Specific Aims:
- To maintain the ED team's high rate of accuracy in data collection
- To begin team participation in corrective action planning
- To improve interdepartmental problem solving
Conclusion
Open communication about errors among all collaborating departments, combing with a shared approach to solving them:
- improved morale and perception of error tracking by the team
- led to a decrease in errors overall, and
- increased interdepartmental collaboration
When all members of the interdepartmental team work together with a positive approach to corrective action, improvement in error rates is a natural outcome of the solutions derived.
-

CLABSI Prevention through Prevention Huddles and CLABSI Risk Assessment and Prevention Form in Electronic Medical Record
Tara Benton, Barb Haney, Lacey Bergerhofer, Yolanda Ballam, and Kaitlyn Hoch
Our aim is to increase the awareness of high risks for central line associated bloodstream infection (CLABSI) and decrease the CLABSI rate with the implementation of CLABSI prevention huddles and an electronic medical record (EMR) "CLABSI Risk Assessment and Prevention" form.
-

Collaboration Between Rheumatology Clinic and Specialty Pharmacy to Positively Impact Patient Experience and Hospital Stewardship
Alaina Linafelter, Julia G. Harris, Robert Herr, Stephanie Quinn, and Ashley M. Cooper
Biologic medications are commonly utilized to treat pediatric rheumatic diseases. Being high-cost, most third-party payers require dispensing through a specialty pharmacy. Children's Mercy Hospital Specialty Pharmacy (CMH SP) started acceting patients in March 2015.
The number of patients benefited by the superior service of CMH SP has risen steadily, leading to high patient satisfaction and financial benefits for the hospital.
-

Decreasing Length of Stay in Pediatric Urgent Care with Electronic Discharge Instructions
Jennifer Wooster, Aimy Patel, Brian R. Lee, and Amanda Nedved
Time spent waiting in the urgent care clinic is dissatisfying for patient and staff. This "wasted time" accounted for more than 52% of the urgent care visit at our urgent care.
The aim of our project is to decrease length of stay by 10 minutes by April 30, 2019 for all patients discharged from Blue Valley Urgent Care by offering patients a paperless depart process. To be eligible for discharge without paper families must be enrolled in the online patient portal.
Electronic discharge instructions significantly decrease length of stay and is associated with improved patient experience scores. Patients who received hardcopy discharge instructions also had short median LOS, likely due to overall improved urgent care workflow with the use of the portal.
-

Development and Implementation of an Evidence-Based Process for Scarce Resource Allocation
Richard K. Ogden Jr., Daniel L. Millspaugh, and Brian O'Neal
Background: Intravenous immune globulin (IVIG) is a plasma-derived product from pooled donors. It has six FDA approved indications. It is also considered standard of care for a few other conditions in specific populations. Additionally, there is growing non-evidence-based use. Due to a global shortage, IVIG has become increasing difficult to obtain.
. . . .
Conclusions: Development, implementation, and promotion of adherence to an evidence-based criterion allowed our scarce IVIG supply to be sustained. Further refinement of the criteria for use is ongoing, as is an evaluation of IVIG utilization by indication, pre- and post-implementation. This process can be applied to other situations of scarce resources
-

Implementing Treat to Target Approach in the Care of Children with Juvenile Idiopathic Arthritis
Julia G. Harris, Jamie Holland, Emily Fox, Leslie Favier, and Ashley M. Cooper
Juvenile idiopathic arthritis (JIA) is the most common chronic inflammatory disease seen in pediatric rheumatology. Despite advances in biologic therapy, many children with JIA will experience morbidity. Treat to Target is a treatment paradigm that involves setting a target of disease activity, using shared decision making, and incorporating clinical decision support. Our clinic aimed to set a treatment target on 50% of eligible JIA patients by December 31, 2019.
-

Improving Bedside Nurse Engagement in Quality Improvement (QI) Projects
Beckie Palmer, Sarah Carboneau, Ashley Domsch, Barb Haney, Brandy Huitt, Ashley Lewis, Ashley Mirabile, Allison Ronco, and Dianne Wilderson
Project Aims:
- Improve nursing engagement in QI as evidenced by increasing nurse involvement to 40% of overall staff by December 2018, with a continual increase to >50% by June 2019.
- Decrease the % of nurses who express "my opinion doesn't matter" as a reason they do not participate in QI by 30% by June 2019.
-
Improving Care of the Small Baby
Beckie Palmer, Abdebayo Oshodi, Brandy Huitt, Kaylee Hurt, Pamela Kliethermes, Trudy Koons, Patricia Lanzer, Ashley Mirabile, Allyson Owen, Christian Anthony Schneider, Betsi Anderson, and Steven Olsen
Hierarchy of Aims:
- Global Aim: Create a Small Baby Unit for infants admitted to our NICU that arebirth, in which 90% of our patients are admitted to F pod on day of admission, by March 2019
- Interim Aim: Staff 80% of our micropremie patients with a Small Baby Team nurse from admission until >32 weeks by May 2019.
- Sub Aim: Increase rates of developmentally appropriate care (2 person cares, kangaroo care compliance) by 50% by August 2019.



