These posters have been presented at meetings in Children's Mercy and around the world. They represent research that was done at the time they were created, and may not represent medical knowledge or practice as it exists at the time viewers access these posters.
-
Improving End Stage Renal Disease Quality Incentive Payment Total Performance Scores
Shelly Guyer, Gina Gregg, and Bradley Warady
The End Stage Rena Disease (ESRD) Quality Incentive Program (QIP) promotes high quality, transparent, cost-efficient care in outpatient dialysis facilities by establishing performance standards that are linked to payment.
The development of a subject matter expert and the sharing of ESRD QIP knowledge resulted in buy-in from dialysis staff and physicians leading to a higher total performance score and the avoidance of payment reduction.
-

Improving Malnutrition Identification in the Outpatient Setting
Kristi Thaete and Karen Stephens
Identification of Pediatric Malnutrition in Outpatient Clinics is the First Step to Allowing Registered Dietitian (RD) Involvement in the Improvement of Patient Care.
-
Improving Pneumococcal Vaccination Rates in High Risk Patients Across Multiple Specialty Divisions
Rachel Moran, Julia G. Harris, Claire Olsen, Rana El Feghaly, Liset Olarte, Douglas Blowey, and Luke A. Harris
Pediatric patients with deficient immune systems or certain chronic medical conditions have an increased risk of acquiring invasive pneumococcal disease.
The 23-valent pneumococcal (PPSV23) vaccine provides protection against 23 pneumococcal serotypes and is recommended for patients aged 2 years or older who are high-risk for invasive pneumococcal disease.
Unfortunately, many high-risk patients are not properly vaccinated due to lack of provider knowledge or understanding of accountability between primary care and specialty providers.
The goal of this project was to improve PPSV23 vaccination rates by 10-20% across multiple Children's Mercy Kansas City specialty divisions.
-

Improving Women, Infants, and Children Participation Using Quality Improvement Methodology
Samuel Little, Sarah Stone, Jeffrey D. Colvin, Sidney Smith, Brenda Hilboldt, Laura Williams, Patricia Marein, Keith Mann, and Kristi Williams
Food insecurity, when a household is unable to acquire food for one or more of its members due to insufficient resources, has recently been on the decline in the United States, according to official 2017 USDA reports.
Unfortunately, this decline has not been observed to the same extent in the demographic of households with children.
WIC is a federal assistance program that works to alleviate the poor health outcomes associated with food insecurity in this demographic by providing eligible, enrolled families with nutritional aid and education.
The specific aim of the project is to increase the percentage of maximum potential WIC appointments that are attended to 85% within 9 months, thus improving nutritional health for eligible individuals within the community.
-

Increasing Kangaroo Care in a New Small Baby Unit
Dianne Wilderson; Barb Haney; Ashley Mirabile; Beckie Palmer; Jenny Heltzer; Erin Keith-Chancy BSN,CCRN; Brooke Smith; Christian Anthony Schneider; and Abdebayo Oshodi
Project Aim: Increase the percent of eligible patients receiving kangaroo care from 19% to 30% by September 2019.
Results:
113 staff completed education
OT consults completed on all SBU patients
20 kangaroo wraps purchased
Kangaroo care rate in NICU increased from 19% (prior to SBU) to 36% (Post SBU opening).
Conclusion: Due to increased multidisciplinary awareness of importance of kangaroo care in the SBU more parents are completing kangaroo care.
-

Increasing Rates of Breastmilk Use at Time of Neonatal Intensive Care Unit (NICU) Discharge: An Improvement Project in a Midwest Level IV NICU
Kathleen Hortenstine, Teresa Fulk, Stephanie Callis, Kyla Galate, and Beckie Palmer
- Breast milk is the preferred food for all infants.
- The rate of breast milk use at time of discharge was below the goal of the institution.
- A gap was identified in bedside nursing education, limiting their ability to provide resources and education to mothers. Nursing involvement ensures skilled, comprehensive, and accessible breastfeeding support.
- The aim of this project is to increase breast milk rates at time of NICU discharge to 95% of eligible patients by December of 2019.
-
Lighting the Way to Ensure Safe Transition Home
Barb Haney, Ashley Mirabile, Dianne Wilderson, Beckie Palmer, Ashley Lewis, Cris Mills, and Eugenia K. Pallotto
All aspects of discharge (education, screenings, appointments, plans and home services" must be completed and appropriately communicated prior to discharge to ensure safe transition to home.
Goal: Standardize all aspects of discharge in a large, busy 84-bed Level IV NICU with >1000 admissions/year and >300 nurses, >60 NNPs, and >25 neonatologists.
- 95% of patients with lengths of stay >3 days have all discharge planning completed prior to discharge/Parent Care Unit overnight stay
-
Making the Management of Acute Otitis Media a SNAP
Cassandra Newell, Donna Wyly, Tanis Stewart, Alaina N. Burns, Brian R. Lee, and Rana El Feghaly
AIM:
To improve Watchful Waiting or Safety Net Antibiotic Prescription (WW/SNAP) in children >6 months old diagnosed with acute otitis media by Advanced Practice Nurses in the Emergency Department by May 2020.
-
Optimizing Antibiotic Management of Pediatric Acute Otitis Media in an Emergency Department
Alicia Daggett, Alaina N. Burns, Brian R. Lee, Nirav Shastri, Patricia Phillips, and Rana E. El Feghaly
Problem
Children diagnosed with acute otitis media (AOM) at the Children's Mercy Hospital Kansas Emergency Department routinely get antibiotic prescriptions. There is rarely discussion with families about watchful waiting (defined as discussion of observation with parents and providing a safety-net antibiotic prescription that parents can ill if the patient is not improving or is worsening over the next 48 hours).
The aim of this quality improvement project is to increase watchful waiting for AOM at the CMK ED by 20% by March 2020, with an overall goal of decreasing antibiotic use for AOM.
-

Pediatric Surgery Opioid Prescription Follow-up
Gadison Quick, Nathaniel Aviles, Gabriel Melgarejo, Hunjung Choi, and Elizabeth Edmundson
This quality improvement project is assisting general and orthopedic surgeons in gaining greater clarity when prescribing opioids for specific surgical procedures. Additional surgical services are being added to the project fall of 2019. Opioid prescribing patterns are, and will continue to be, key to all prescribing providers within our organization.
-
Safe Sleep in the NICU
Ashley Mirabile, Barb Haney, Dianne Wilderson, Beckie Palmer, Ashley Domsch, and Eugenia K. Pallotto
Goal: To evaluate a staff education program on approach to improve in the rate of eligible NICU infants in safe sleep in a busy 84-bed level IV NICU.
Outcome Measures; Improve safe sleep compliance for eligible patients to 90% or greater by December 2019.
Process Measures: Audits from bedside RNs showing compliance with safe sleep.
Planned Intervention: In December of 2018 a multidisciplinary work group brainstormed and implemented best practice safe sleep education for staff and parents. September 2019 a Safe Sleep Educational Toolkit was made available for staff.
Results: Safe Sleep compliance has gone from 53% to 90% in September of 2019 after the initiation of a safe sleep toolkit.
-
Safe to Sleep in the ICN
Megan Kelly, Alexandra (Lexi) Van Noy, Molly Kruse, Megan English, Hannah Culbertson, Brianne Truitt, Ziryan Salihparkhy, Jenny McKee, and Brecklyn Findley
The CDC states that 1,545 infants passed away from SIDS in 2014. Safe sleep includes supine, in a crib, head of bed flat, firm sleep surface, tightly fitted sheet, no loose blankets, no toys or supplies in crib with infant. It is important for nurses to model safe sleep practices in the hospital setting. Current compliance with safe sleep in the Intensive Care Nursery is 50%.
AIM Statement:
By August 1, 2019 we want to increase the compliance of modeling safe sleep behaviors for patients who qualify for safe sleep from 50% to 90% in the Intensive Care Nursery.
-
The Kanga-Croo: Nurse Resident Champions Creating Momentum for Improvement
Brett Butler, Jacob Burden, Carly Creekmore, Blair Griffin, Taylor Godemann, Taylor Hagen, Theresa Koelling, Mary Anne Kucera, Halle Magid, Makenna Miller, Monica Page, Mary Riffel, Madison Stebbins, Sarah Stokes, and Skylar Suppes
Topic Summary:
Kangaroo Care (skin to skin care) is a parent-led, evidence-based intervention which improves outcomes in neonatal patients including: decreased apnea, increased weight gain, increased parent satisfaction and decreased length of stay.
Results:
Nurse resident team interventions to support parent engagement and remove barriers to Kangaroo Care (KC) through iterative PDSA cycles from January 2018 to July 2019 yielded positive results within a subset of ICN patients.
-

Trauma Informed Care: Improving Staff Morale on 6 Henson
Kara Humphreys, Katherine Karstens, Kortney Neiderhauser, Briana Pina, Payton Tallent, Stephanie Assad, and Madison Dexter
Six Henson staff reported feeings of burnout and compassion fatigue.
Aim Statements:
Decrease percentage of 6 Henson staff feeling sometimes or often "worn out because of [their] work as a helper" from 86% to 50% by August 1, 2019.
Increase the number of KUDOS cards submitted by 6 Henson staff from 2-3 per week to 10 per week by August 3, 2019.
Both aim statements were met and exceeded.
-

Using a Standardized Admission Handoff (I-PASS) to Improve Communication Between Pediatric Urgent Care and Inpatient Providers
Amanda Nedved, Kathleen Berg, and Amanda Montalbano
Ineffective hand-off communication is recognized as a critical patient safety problem in health care. A pre-interventions survey of pediatric urgent care providers and pediatric hospitalists demonstrated an opportunity for improvement of communication during admission handoffs.
Standardized handoffs improve communication without impeding provider workflow. We learned that subjective terms for illness severity ("stable," "watcher," and "unstable") did not translate well from urgent care to inpatient. We are planning on implementing an objective standardized tool (PEWS) to improve the communication of illness severity. We have also updated the I-PASS visual aid based on feedback.
-

"Will Using Telemedicine with Medical Command during Situational Awareness Escalation Add Value to Patient Care?"
Kathy Farrell, Bradley Bishop, Lisa Carney, Matthew B. Johnson, Natalie Masters, Lisa Pruitt, Sherry McCool, and Laura Fitzmaurice
-

Thyrotoxicosis Presenting with Nondiabetic Ketoacidosis in a 4 Year Old Female: A Case Report
Henry S. Jeng, Michelle Knoll, and Figen Ugrasbul
Objective: To raise awareness that thyrotoxicosis should be on the differential diagnosis for ketoacidosis in the pediatric population
-

Health Literacy Challenges and Opportunities: Bringing Children’s Mercy and Kansas City Together
Jennifer A. Lyon, Angie Knackstedt, Barbra Rudder, Mamta Reddy MD, and Courtney R. Butler
BACKGROUND: A multidisciplinary group at Children's Mercy Kansas City applied for and received the NNLM MCR's Immersive Workshop Grant in December, 2017, and used the funding to organize and host a two-day immersive, interprofessional workshop in April, 2018, that 1) brought together health literacy-invested groups and individuals within the Kansas City community to learn about health literacy including cultural, language, numeracy and digital inclusion factors; and 2) provided specialized training to targeted CM participants to improve the provision of bedside health information to patients and caregivers. Objectives included: increasing community-wide collaboration, sharing resources, encouraging participants to become change agents, and strategizing organizational initiatives. DESCRIPTION: The project team consisted of 2 librarians, a practicing physician, a child life specialist, and a nurse educator specializing in equity and diversity; all were past or present members of the institution's Health Literacy Committee. Day One, at the Public Library, was open to the community. Over 25 organizations involved with health literacy and health equity were invited to contribute speakers and participants. Dr. Ruth Parker of Emory University delivered two 'keynote' lectures. Other speakers represented an adult literacy volunteer agency, the Public Library, and an immigration support organization. Day Two was held internally, focusing on hospital employees professionally invested in promoting health literacy practices in patient care. Additional training on institution-specific resources was supplemented by interactive, hands-on practice sessions and brainstorming exercises intended to develop internal health literacy pilot projects, with encouragement to reconnect with the community organizations. CONCLUSIONS: Day One had 73 attendees (28% from the community). Day Two had 60 attendees. All participants were fully engaged throughout, including interactive brainstorming activities. All informal comments to organizers were positive and the planning team has received requests to repeat the workshop in the future. A survey was sent to all attendees (67-69% response rates). On a Likert scale from 1-5, the means on questions regarding health literacy awareness, motivation to take action, and increased knowledge of resources and collaboration opportunities ranged from 4.88-4.95 for both days. Internal projects are being developed and communication with external groups has steadily increased.
-
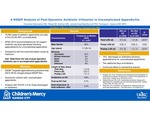
A NSQIP Analysis of Post-Operative Antibiotic Utilization in Uncomplicated Appendicitis
Charlene Dekonenko, Robert M. Dorman, Janelle R. Noel-Macdonnell, and Tolulope A. Oyetunji
APSA 2010 recommendations do not support antibiotic use post-operatively following appendectomy for uncomplicated appendicitis, but compliance varies by institution. This study determined the rate of post-operative antibiotic use in uncomplicated appendicitis and found that 10% of patients were discharged on antibiotics, using the NSQIP files.
-

A Review of First Year Fellow Endoscopic Skills and Time to Proficiency
Antoinette Adjowa O. Walker, Dalya El Tawil, Jennifer Colombo, Nicholas Clark, and Kimberly J. Reid
Through this quality improvement project, we have assessed the current fellows' upper endoscopy skill level during their first year and determined that the time to achieving proficiency is significantly longer than desired. The goal is to prepare new fellows for endoscopy prior to the beginning of their rotations with a curriculum that includes assigned reading materials, videos, and simulated endoscopic cases, to promote safety and increase satisfaction of patients by improving the readiness, skill level, and the confidence of first year inexperienced fellows.
-
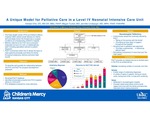
A Unique Model for Palliative Care in a Level IV Neonatal Intensive Care Unit
Kelstan L. Ellis DO, Megan Tucker, and Jennifer Linebarger
This poster describes a review of the relationship between the Fetal Health Center and the Palliative Care team as the Palliative Care Team follows the patient family from prenatal through neonatal intensive care.
-

AV Nodal Reentrant Tachycardia in Patients with Twin AV Nodes
Christopher Mathis, Svjetlana Tisma-Dupanovic, Lindsey Malloy-Walton, and John Papagiannis
-

Dehydrated Hereditary Stomatocytosis Causing Sever Ascites Leading to Pulmonary Hypoplasia and Respiratory Insufficiency in a Neonate
Michael D. McDowell Jr and Christopher M. Oermann
Care Presentation: EM is a 32.5-week EGA infant who was born with sever congenital ascites (following repeated prenatal paracentesis) identified on prenatal ultrasound. Initial chest-abdomen imaging is shown in Figure 1. He required CPAP at delivery but was weaned of high flow nasal cannula with intermittent episodes of prolonged intubation during repeat paracentesis. Paracentesis demonstrated simple ascites rather than chylous fluid. Lymphangiograms demonstrated transient lymphatic leakage with resolution. Genetic evaluation revealed a pathogenic mutation in the PIEZO 1 gene for autosomal dominant DHS. This disorder had reduced penetrance and variable expressivity and symptoms range for absence of clinical features to lethal perinatal edema. During his first year of life EM developed severe chronic obstructive pulmonary disease with hypoxemia and a requirement for supplemental oxygen, restrictive lung disease secondary to thoracic dystrophy, and chronic lung disease of prematurity. He remained on supplemental oxygen for the first year and a half of life. Discussion: DHS is a rare form of autosomal dominant hemolytic anemia reported in 26 individuals among 7 families worldwide. Clinical presentation varies significantly and includes chronic anemia, neonatal edema and ascites, and lymphatic malformations. Symptoms may develop in utero, during the perinatal period , or later in adulthood. Pulmonary hypoplasia and respiratory insufficiency caused by pre/perinatal ascites have not been reported. DHS is caused by gain-of-function mutations in the PIEZO1 (16q24.3) gene, as was demonstrated in our patient. Mutations result in increased red cell cation membrane permeability, particularly potassium, leading to depletion, dehydration, and shortened red cell survival. Expression of PIEZO1 in lymphatics may explain pre/perinatal edema and ascites. EM developed sever prenatal ascites leading to abnormal abdominal musculature and impaired diaphragm movement and fetal breathing causing pulmonary hypoplasia with subsequent respiratory insufficiency at birth. The pathophysiology in this case is similar to that of prune belly, where abnormal abdominal musculature is known cause of impaired lung growth and development and subsequent respiratory compromise. Respiratory complications are primarily managed with supplemental oxygen and ventilatory support, if needed, until the lungs mature. Conclusion: This case highlights a previously unreported extremely rare disease, DHS, leasing to abnormal fetal breathing , marked pulmonary hypoplasia, and subsequent respiratory insufficiency.
-

Does Pediatric Palliative Care Involvement Influence Location of Death?
Joy Solano, Meghna Singh, Ashley K. Sherman, and Jennifer Linebarger
This study describes the influence of a palliative care team on location of death and location of death discussions with patients/caregivers, and determines whether location of death discussions influence location of death.
With palliative care or a location of death discussion, patients were less likely to die in the PICU and more likely to die at home. Location of death discussions were more likely to occur if a palliative care team was involved.
-

Fetal Ventricular Measurement in Determination for Intrauterine Closure of Myelomeningoceles
Paige Lundy, Emanuel Vlastos, and Paul A. Grabb
Prenatal closure of myelomeningoceles for fetuses with ventricular width of greater than 15 mm at the time of intrauterine screening (19-25 weeks) has been discouraged, but little is documented regarding the details of ventricle measurement, modality, and timing. This study concludes that ultrasound and MRI provide different results in regards to fetal ventricle size. If treatment recommendations are going to be offered or withheld based on the 15 mm "rule" the method of fetal imaging must be taken into account.



