These posters have been presented at meetings in Children's Mercy and around the world. They represent research that was done at the time they were created, and may not represent medical knowledge or practice as it exists at the time viewers access these posters.
-

Gonadotropin Releasing Hormone (GnRH) Agonist Improves Hyperandrogenism in an Adolescent Female with a Novel Insulin Receptor Gene Mutation
Emily Paprocki, Romina Barral, Heidi Vanden Brink, Maria E. Lujan, and Tania S. Burgert
We describe a case of an adolescent female with Type A insulin resistance whose severe hirsutism and hyperandrogenism were improved with leuprolide, despite extreme hyperinsulinemia. Ovarian volume decreased in association with the resolution of hyperandrogenism, consistent with ovarian size reflecting hyperandrogenism in adolescents.
This case allowed us to examine the frequently debated bidirectional relationship between insulin and hyperandrogenism, often deemed independent of gonadotropin activity.
-

Improving NICU Referrals to the Missouri Early Intervention Program (First Steps)
Luke Prest, Lauren Fenstermann, and Ayman Khmour
First Steps is the statewide early intervention program in Missouri, but a review of referrals from the Truman neonatal intensive care unit revealed that only 24% of eligible patients were being referred. This poster describes efforts to increase awareness among residents and to refer all eligible patients to First Steps upon discharge.
-

Neuroblastoma in Adolescents and Children Older than 10 Years: Unusual Clinicopathologic and Biologic Features
Laura McCarthy, Katherine Chastain, Terrie Flatt, Eugenio Taboada, Robert E. Garola, John Herriges, Linda D. Cooley, and Atif Ahmed
This poster describes four cases of neuroblastoma diagnosed since 2008 in children greater than 10 years and presents their clinical, histologic and biologic features, emphasizing unusual clinicopathologic characteristics and the role of DNA microarray analysis and Next Generation Sequencing in their management.
-

Outcomes Following Dynamic Compression Bracing for Pectus Carinatum
Charlene Dekonenko, Robert M. Dorman, Amy L. Pierce, Beth A. Orrick, David Juang, Pablo Aguayo, Jason D. Fraser, Tolulope A. Oyetunji, Charles L. Snyder, Shawn D. St Peter, and G W. Holcomb III
We describe our experience with dynamic compression bracing for pectus carinatum patients and their satisfaction with bracing.
-
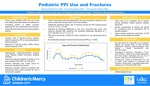
Pediatric PPI Use and Fractures
Nathan R. Fleishman, Troy Richardson, and Thomas M. Attard
This study compared the rate of fracture among pediatric patients exposed to proton pump inhibitors to the rate among patients without exposure, and also considered the fracture location among children exposed to proton pump inhibitors.
-

Predictive Performance of Existing Population Pharmacokinetic Models of Tacrolimus in Pediatric Kidney Transplant Recipients
Alenka Chapron and Susan M. Abdel-Rahman
With the goal of developing a clinician-driven tacrolimus (TAC) pharmacokinetic dosing tool, our initial objectives were 1) to examine whether published TAC population pharmacokinetic (popPK) models could serve as a foundation for the dosing tool, and 2) evaluate their performance predicting TAC concentrations in an independent cohort of Children's Mercy patients.
-

Prospective Evaluation of a Population Pharmacokinetic Model of Pantoprazole for Obese Children
Alenka Chapron, Susan M. Abdel-Rahman, and Valentina Shakhnovich
We previously developed a population pharmacokinetic (popPK) model of pantoprazole for obese children. Our objective was to evaluate the predictive performance of this model in an independent cohort of normal weight, overweight and obese children.
-

Quality Improvement: Implementing a Foot Exam to Improve Care for Patients with Diabetes Mellitus
Emily Paprocki, Ryan McDonough, Tiffany Musick, and Joseph Cernich
The American Diabetes Association guidelines recommend an annual foot exam in patients with type 1 and 2 diabetes who are ten years old or older and who have been diagnosed with diabetes at least five years. Quality improvement tools were used to improve the care provided to our patients by implementing an annual food exam.
-

Self-Reported Outcomes Following Cholecystectomy for Pediatric Hyperkinetic Biliary Dyskinesia
Charlene Dekonenko, Joseph A. Sujka, Robert Michael Dorman, Tolulope A. Oyetunji, and Shawn D. St Peter
The aim of this study is to determine if children with hyperkinetic biliary dyskinesia have resolution of symptoms after laparoscopic cholecystectomy at our institution.
Conclusion: Cholecystectomy for hyperkinetic biliary dyskinesia may or may not improve symptoms. Further research should focus on pathophysiology of the disease in order to create an evidence-based definition of biliary dyskinesia in children to determine who will benefit from cholecystectomy. -

The Effect of Antihypertensive Dosing on Hypertension in Children with Chronic Kidney Disease
Benjamin A. Matta, Uri S. Alon, Tarak Srivastava, Bradley A. Warady, and Darcy Weidemann
This study's objective was to determine the effect of antihypertensive dose on hypertension status in children with chronic kidney disease. This was the first quantitative analysis of antihypertensive dose expressed as a newly developed measure, cDDI, and is relationship with hypertension status in children with CKD.
-

Viral Whole Genome Sequencing for Antiviral Resistance in a Child with DOCK8 Deficiency and Recurrent HSV-1
Sean Stout, A. L. Greninger, Rangaraj Selvarangan, A. F. Freeman, Brandon D. Newell, Erin Stahl, and Dwight Yin
We present the case of a child with dedicator of cytokinesis 8 (DOCK8) deficiency and chronic, resistant HSV-1 mucocutaneous infections to illustrate the clinical utility of viral whole genome sequencing to detect active and latent HSV resistance mutations.
-
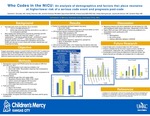
Who Codes in the NICU: An Analysis of Demographics and Factors that Place Neonates at Higher/Lower Risk of a Serious Code Event and Prognosis Post-Code
Danielle N. Gonzales, Ashley K. Sherman, Jennifer Dremann, Staci Elliott, Amelia Gute, Amber Bellinghausen, Jessica Brunkhorst, and Danielle Reed
This study analyzed resuscitation events in a level IV neonatal intensive care unit from 2012-2017 to determine whether there are identifiable differences between those who have a rapid response event and those with a short or long code and determine factors post-event that may impact survival to discharge.
-

Improving Discharge Communication with Outpatient Providers on the Hospitalist Service
Nicholas Clark, Julia Simmons, Angela Etzenhouser, Troy Richardson, Patrick Brady, and Eugenia K. Pallotto
Describes a quality improvement project to increase two-way discharge communication between pediatric hospitalists and primary care providers from 7% to >80% within 18 months.
-

Practice Variations in Sedated Echocardiography and Impact on Repeat Echocardiography in Non-Refractory Kawasaki Disease
Nicholas Clark, Troy Richardson, Jennifer E. Schuster, Anitha Parthiban, and Henry T. Puls
This study discovered significant variation among children's hospitals in the use of sedated echocardiiography for children <30 months of age with non-refractory Kawasaki disease prior to the American Heart Association 2017 Kawasake disease guideline update. Consideration should be given to performing sedated echocardiography as it may reduce the need for repeat echos without impacting length of stay or total>costs.
-

The Effect of Antihypertensive Dosing on Hypertension in Children with Chronic Kidney Disease
Benjamin A. Matta, Uri S. Alon, Bradley Warady MD, Tarak Srivastava, and Darcy Weidemann
Background
Hypertension (HTN) is a highly prevalent and major risk factor for poor cardiovascular and renal outcomes in chronic kidney disease (CKD). Previous research suggests that HTN is underdiagnosed and undertreated in children with CKD. To our knowledge no studies have investigated the effect of antihypertensive (antiHTN) dose on blood pressure (BP) control in this population.
Objective
To determine the effect of antiHTN dose on HTN status in children with CKD.
Methods
Study population: 255 participants studied in the Chronic Kidney Disease in Children (CKiD) study at their 3rd visit, taking at least 1 antiHTN drug.
Cumulative Drug Dose Index (cDDI): We developed a new quantitative tool, Drug Dose Index (DDI) which is expressed as a ratio between the current dose and the maximum potential dose, accounting for age, weight and renal dose adjustments. cDDI = sum DDI for all antiHTN agents for a subject.
Primary outcome: HTN status - controlled HTN (cHTN) or uHTN (= masked HTN or ambulatory HTN).
Secondary outcome: Left ventricular hypertrophy.
Statistical analysis: Univariate analysis: Comparison of cDDI between the outcome groups. Multivariate Logistic Regression: 2 models with outcomes: uHTN and LVH.
Results/Discussion
This was the 1st quantitative analysis of antiHTN dose (cDDI), and its relationship with HTN status in children with CKD. No differences in cDDI between uHTN vs. cHTN, or LVH vs. no LVH, but higher cDDI was associated with AH on univariate analysis. RAASi and diuretic use were associated with lower odds of uHTN. Non-Caucasian race, absence of RAASi and diuretic agents, and higher number of agents were associated with uHTN. Female gender, higher BMI z-score, lower eGFR, higher number of agents and lower cDDI were associated with LVH. Further research is needed to validate the use of cDDI and the the roles of medication class and dose on BP control in children with CKD.
-

Improving bronchiolitis care across multiple care settings using a deimplementation bundle
Amanda Nedved, Kathleen Berg, Troy Richardson, Amanda Montalbano, and Matthew B. Johnson
Despite the availability of a bronchiolitis CPG; variation in care practices still existed at our institution. The aim of our quality improvement (QI) project was to increase overall adherence with our institutional CPG in patients 60 days to 24 months of age diagnosed with bronchiolitis in the urgent care centers (UCC), emergency departments (ED), and general inpatient units from a baseline of 40.9% to 60% by the end of two bronchiolitis seasons.
-

Total and Free Plasma Bilirubin and Clinical Outcomes in Severe Hyperbilirubinemia
Sean M. Riordan, Jean-Baptiste LePichon, Steven Shapiro, Tina Slusher, Fatima Abdullahi, Hafsat M. Suleiman, Victor C. Pam, Mamu B. Samuel, Christopher S. Yilgwan, Christian Isichei, and Idris Y. Mohammed
Acute bilirubin encephalopathy (ABE) and kernicterus spectrum disorder (KSD) have become relatively uncommon in high income countries but remain a major cause of morbidity and mortality in low- and middle-income countries. To better understand the relationship between free (Bf) and total (TB) bilirubin levels and the development of ABE and KSD we followed infants born in three large tertiary centers in northern and central Nigeria (Jos, Kano and Zaria).
-

Weighted Pathway Genetic Load Analysis of Hyperbilirubinemic Infants Indicates a Potential Genetic Component for Susceptibility to Bilirubin Neurotoxicity
Sean M. Riordan, Jean-Baptiste LePichon, Steven Shapiro, John Cowden, Monica VillaGullen, Laurence Thielemans, Dina Villanueva Garcia, and Jesus Aguirre-Hernandez
Severe kernicterus spectrum disorder (KSD) is described as motor and auditory deficits resulting from brain damage caused by hyperbilirubinemia. The severity of HB does not always predict the severity of injury. The lack of a strong monogenetic link to susceptibility suggests bilirubin-induced brain damage may be due to impaired bilirubin response pathways. This poster describes work to use a modified pathway genetic load (mPGL) score method to perform a targeted genetic analysis of whole exome data from patients with various degrees of neonatal HB, with an ultimate goal of developing a neonatal screen to susceptibiltiy to bilirubin neurotoxicity.
-

Developing Technologically Advanced Research in Low- and Middle-Income Countries
Isa Abdulkadir, Tina Slusher, Fidelia Bode-Thomas, Sean Riordan, Jean-Baptiste LePichon, Laila Hassan, Shehu Abdullahi, Akinyemi Ofakunrin, Stephen Oguche, Steven Shapiro, and William Ogala
This poster presents a collaboration between a group of scientists in Nigeria and the USA in developing a genomic research project and the solutions adopted in tackling the ethical implications and partnership equity and ownership of such a project.
-

Identifying Structural Factors Associated with Central Line-Associated Bloodstream Infections (CLABSI) Risk in a Single-Center Pediatric Academic Hospital
Elizabeth Monsees, Paul N. Bauer, Yolanda Ballam, and Brian R. Lee
Objective: compare unit structure and process-related factors against unit-specific CLABSI rate.
Conclusion: CLABSI mitigation requires more than individual competence with task-related practices; the unique work ecology of each clinical area may broadly influence CLABSI as an outcome; extending analyses to consider organizational structure can inform resource allocation and recalibrate traditional prevention strategies.
-

Sepsis: Triage Triggers, Outcomes Quicker
Rylee Ainge, Mackenzie Flaws, Natalie Heim, Emily Herndon, Hayley Norris, and Amy L. Scott
-

Analgesia and Sedation Medication Use in Infants with Congenital Diaphragmatic Hernia is Associated with Adverse Outcome
Mark Weems, Theresa Grover, Robert DiGeronimo, Jason Gien, Ruth Seabrook, Sarah Keene, Natalie Rintoul, Beverly Brozanski, John Daniel, Rachel Chapman, Burhan Mahmood, Yvette Johnson, Yigit Guner, Holly Hedrick, Isabella Zaniletti, and Karna Murthy
This study describes the use and variation of sedation and analgesic medications as well as short-term clinical outcomes in infants with congenital diaphragmatic hernia.
-

Association of Food Deserts and Pediatric Hospitalization Rates
Laura Plencner, Matthew Hall, Molly Krager, Henry T. Puls, Jessica L. Markham, Ellen Kerns, and Jessica L. Bettenhausen
Retrospective cross-sectional study describes differences in hospitalization rates for children based upon their residence within a food desert and describes any differences among reasons for hospitalization.
-

Burnout and Resilience Among Pediatric Residents in Stockholm, Sweden: Findings from a Mixed-Methods Study
Lauren Poull, Sanaz Skyttner-Rahmani, Andrea P. Anderson, Weston T. Powell, Jiaqi Yin, Carolyn C. Foster, and Maneesh Batra
Objective
To measure the prevalence of burnout among pediatric residents at Karolinska University Hospital (KUH).
To describe the local drivers of burnout and the protective factors that lead to resilience and workplace engagement.Conclusions
Prevalence of burnout among Swedish pediatric residents in this study was 39%, which is lower than reported in the US (50-60%).
Drivers of burnout were identified across all four domains. They included local features of the learning environment, and many are modifiable.
Protective factors include perceived control over scheduling, better mental and physical health, lower perceived stress, and being a parent.
Future work will evaluate interventions designed to modify the drivers of burnout and reinforce the drivers of resilience. -

Chenla Children's Healthcare in Kratie, Cambodia
Clayton Mowrer
Describes a global health learning experience in Kratie, Cambodia.



